Pediatric Concussions - Babies, Toddlers, and Children
If your child has sustained a concussion, this page can help you manage your baby, toddler, or child's concussion recovery. Better understanding what your child is going through can improve their recovery from concussion.
Contents
How to Recognize Signs and Symptoms
Infants (0-1 year) | Toddlers (2-4 years) | Elementary age (5-12 years)
Most Common Causes of Concussion
When to see a Healthcare Provider
Recommended timeframe to meet a provider | What to do at the provider
When to Check back with the Doctor
Recognizing when symptoms become persistent | What to do about persistent symptoms
Evidence-based Steps for Recovery
A parent’s role in their child’s recovery | Overparenting
The role of a school professional | How teachers can support return-to-school
The mental health of concussed children | Helping your child maintain social connections
Recognizing Signs and Symptoms
All concussions present different signs and symptoms. There are many things to look for when diagnosing concussions, and symptoms may not appear for hours or even days after the initial injury. Dr. Susan Klein stated that the five standard categories of concussion symptoms are balance problems, sleeping problems, headaches, problems with thinking, and emotional alterations.
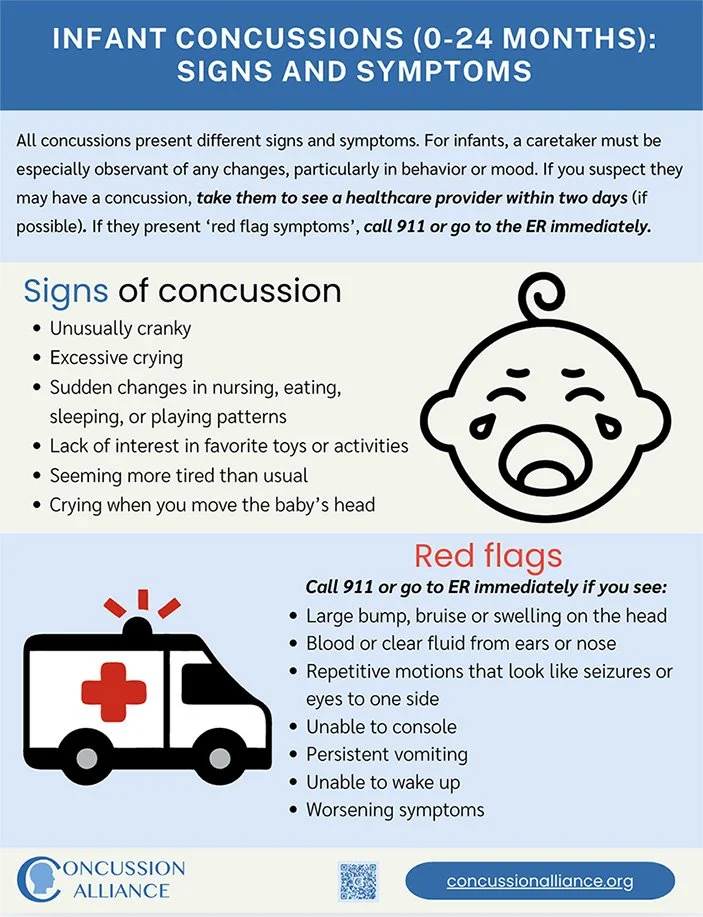
Infant (0-1) Signs and Symptoms
Concussions in infants and babies are especially difficult to diagnose because they cannot communicate like older children. It is important to watch for any behavioral changes or changes in appearance. If you have any concerns that your baby may have sustained a concussion, it is always a good idea to visit a healthcare provider and talk to them about the nature of the injury. Like any other population, concussions will have different signs and symptoms in babies.
Signs of concussion to watch for in an infant include:
Crankiness and irritability (beyond their usual)
Cannot be comforted or excessive crying
Sudden changes in nursing, eating, sleeping, or playing patterns
Lack of awareness or perception
Lack of interest in favorite toys or activities
Seeming more tired than usual
Crying when you move the baby’s head
Red Flag signs and symptoms (Call 911 or go to the emergency room immediately)
Large bump, bruise or swelling on the head
Blood or clear fluid from ears or nose
Repetitive motions that look like seizures or eyes to one side
Unable to console or calm
Unable to wake up
Persistent vomiting
Worsening symptoms
We recommend you visit UCSF Benioff Children's Hospital concussion guide for infants and toddlers to learn more about concussions in babies.
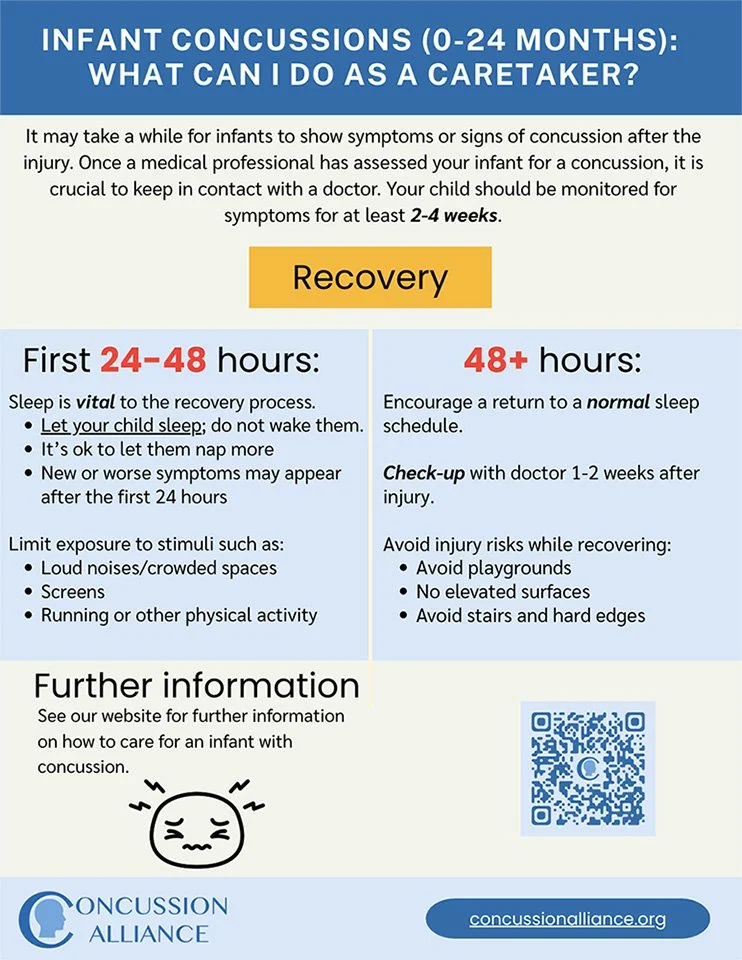
Click here or on the images below to download our PDF about infant concussions
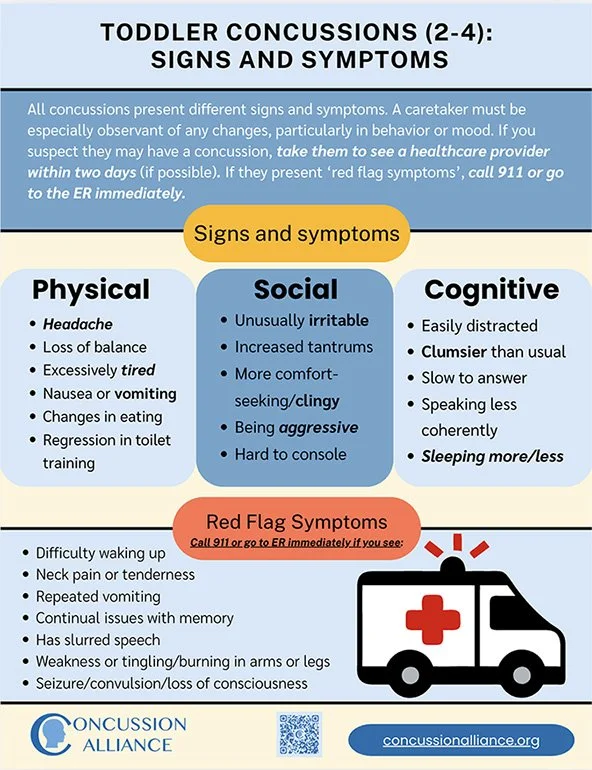
Toddler (2-4 years old) Signs and Symptoms
Physical
Headache
Sensitivity to noise and light
Loss of balance
Trouble walking
Being excessively tired or drowsy
Nausea or vomiting (repeated vomiting is a red flag–take your child to the ER)
Vision changes
Thinking and concentrating
Trouble thinking clearly
Trouble remembering
Slow to answer questions
Speaking less coherently than usual
Trouble recalling events before or after concussion
Social and emotional
Being irritable or fussier than normal
Feeling more emotional
Feeling sad or nervous
Being aggressive
Hard to console
Sleep
Sleeping less than normal
Sleeping more than normal
Trouble falling asleep
Red Flag signs and symptoms (Call 911 or go to emergency room immediately)
Neck pain or tenderness
Difficulty waking up
Repeated vomiting
Continual issues with memory
Has slurred speech
Weakness or tingling/burning in arms or legs
Cannot recognize people or places
Seizure or convulsion
Loss of consciousness
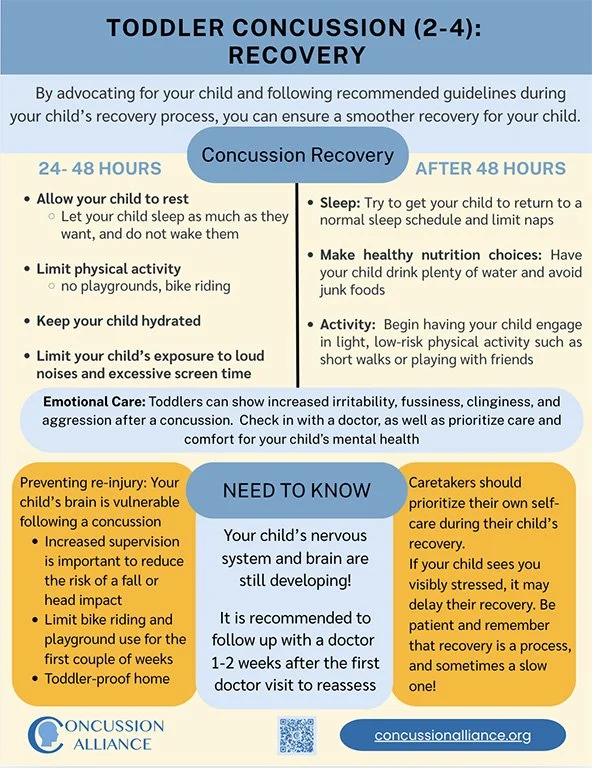
Click here or on the images below to download our PDF about toddler concussions.
Elementary age (5-12) Signs and Symptoms
Physical
Headache
Sensitivity to noise and light
Loss of balance
Being excessively tired or drowsy
Nausea or vomiting
Vision changes
Unsteadiness when walking
Fatigue
Thinking and concentrating
Slow to answer questions
Trouble recalling events before or after concussion
Tires when attempting cognitive tasks
Refuses to read or do work
Inconsistent performance in school
Difficulty concentrating
Difficulty remembering and memorizing
Distracting easily
Disorganization
Difficulty learning new information
Social and emotional
Irritable and/or angry
Depressed
Feeling more emotional
Aggressiveness
Motivational issues
Wanting to socially isolate
Anxiety
Sleep
Sleeping less than normal
Sleeping more than normal
Trouble falling asleep
Red Flag Symptoms (Call 911 or go to emergency room immediately)
Neck pain or tenderness
Double vision
Weakness or tingling/burning in arms or legs
Severe or increasing headache
Seizure or convulsion
Slurred speech
Loss of consciousness
Deteriorating conscious state
Repeated Vomiting
Trouble waking up
We recommend the CDC and CATTonline as additional resources for signs and symptoms of concussion.
Click here or on the images below to download our PDF about toddler concussions.
Most common causes of concussion
Visual created by Beckett Schafer (2022 Concussion Alliance Winter Extern)
Falls
The most common cause of concussion in children are falls.
A fall at ground level can absolutely cause a concussion.
Children 0-4 are most at risk for falls
Falls account for more than 70% of Traumatic Brain Injury related ED visits in this age group
Blunt Force Trauma
A blunt force injury is when an object hits someone or someone collides into an object
Blunt force trauma are the second most common cause of concussion in children
Blunt force trauma accounts for 35% of Traumatic Brain Injury in ages 5 to 14.
Abuse
Abuse is another leading cause of Traumatic Brain Injury (TBI) and concussion, especially in young children
These injuries are often undiagnosed
Children with concussions from abuse are less likely to get proper care than those who have sustained concussions other ways
Sports
Older children are more likely to sustain a sports-related concussion
Once a child sustains one concussion, they are more likely to sustain another
Some sports have higher concussion rates than others, but most have some risk of player-to-player impact or falls
Car Accidents
Always drive safely, especially when your child is in the car with you
Children are most likely to die from TBI resulting from car crashes than from any other cause
For more on causes of concussion in children visit the CDC's report to congress on TBI in children.
How to reduce risks
Ways to reduce the risk of concussions for your child:
Safety in cars: When traveling in a car, always buckle your child in a correctly installed car seat, booster seat, or seat belt that is appropriate for your child’s age and size.
Helmet safety: Make sure that your child is wearing a well-fitting helmet and other protective gear when riding bikes or scooters, skateboarding, or snowboarding. Note: helmets don’t prevent concussions, but they can soften some forces to the head and are critical in preventing more serious head injuries like skull fractures.
Stair gates: Use gates to block off access to risky areas such as stairs, high counters, and tall and heavy furniture your infant or toddler may try to climb to prevent serious falls.
Soft surfaces: Use playgrounds with soft material under them, like mulch or sand, instead of grass or dirt, to reduce impact and avoid injury during falls.
Be attentive: Never leave your child unattended; closely supervise their play, especially during recovery.
When to see a healthcare provider
If you observe signs or symptoms of a concussion in your child, take them to see a healthcare provider in a clinic within 24 to 48 hours of the injury. If you are unable to visit a healthcare provider in person, telemedicine and telehealth services are also options. Learn more about Telehealth.
If you observe any of these “red flag” danger signs in your child, seek care immediately at an emergency department.
Loss of consciousness
Increasing confusion or becoming drowsy and less responsive
Seizures/convulsions
Slurred speech
Severe or increasing headache
Weakness or tingling/burning in the arms or legs
Being increasingly agitated/combative
One pupil is larger than the other
Vision loss or double vision
Repeated vomiting
Will not stop crying and cannot be consoled
Will not nurse or eat
At the healthcare provider
Inform your healthcare provider about any prescription, over-the-counter medicines, or natural remedies your child uses.
Write down and share the following information with your provider:
Cause of the injury and force of the hit or blow to the head or body
Any loss of consciousness (passed out/knocked out), and if so, for how long
Any alteration of consciousness (feeling dazed, confused, not quite themselves right away)
Any memory loss right after the injury
Any seizures right after the injury
Number of previous concussions (if any)
Why didn’t the doctor order a brain scan?
Be informed about scans: Considering that concussions do not show up on CT or MRI scans, and the effects of radiation on young children whose brains are still developing, doctors don’t typically order these scans. A CT or MRI will be ordered only if the doctor suspects bleeding in the brain or another type of more severe head injury, such as a skull fracture. However, they use a range of assessment tests to check for concussion symptoms related to cognition, memory, balance, visual processing, and more.
At the end of the appointment, get written discharge education and, if applicable, return to play instructions for your child.
When to check back with the doctor
PedsConcussion recommends a follow-up 1-2 weeks after your child’s initial visit “to re-assess and monitor clinical status.” The guideline also recommends an immediate follow-up if your child gets worse.
Re-visit a provider if your child has any of the following signs or symptoms:
Increased confusion
Worsening headache
Vomiting more than once
Seizures
Not waking up
Trouble walking
Difficulty talking
Strange behavior
If your child is experiencing neck problems or dizziness, request a referral to physical therapy as soon as the first week.
If recovery takes longer than 28 days, visit a provider to identify potential factors for prolonged recovery, and for referrals to multidisciplinary care.
Persistent Symptoms
For a majority of children, concussion symptoms subside within 2-4 weeks, but sometimes symptoms last beyond the average recovery time of one month. A commonly used term for this is post-concussion syndrome (PCS), and researchers now use the term “persisting symptoms after concussion (PSaC). See our Persisting Symptoms resource to learn more.
A 2022 study found “The prevalence of [persisting symptoms] among children after mTBI is not well known, with reports ranging from 2.3 to 33%.”
PSaC symptoms can include headaches, dizziness, sleep problems, difficulties with concentration and memory, mood or anxiety problems, and difficulty tolerating school or exercise.
A 2022 research study found that fatigue and headache were the most common symptoms children reported 28 days after their injury. The most commonly reported co-occurring post-concussive symptoms were fatigue, headache, and difficulty concentrating.
The figure lists the four common groups of persistent symptoms. Persistent symptoms require multidisciplinary rehabilitation. Visual created by Jemsy Mathew (2022 Concussion Alliance Winter Extern)
What to do about persistent symptoms
When symptoms persist beyond expected time frames, multidisciplinary rehabilitation is necessary. This is a breakdown of common persistent symptoms and corresponding treatments:
Post-traumatic headache
Concussion Alliance has two pages that extensively cover different kinds of headaches and their treatments: Headaches, and Headaches: Advanced Page. Research shows that cognitive behavioral therapy (CBT) is effective for post-concussion headaches in children. See our resource Cognitive Behavioral Therapy.
Concussion Alliance would like to point out that there is some (limited) evidence for craniosacral therapy and acupuncture for persistent concussion symptoms, and members of our community have found both to be helpful and easily accessible treatments. See our pages on Craniosacral Therapy and Acupuncture to learn more.
Vestibular-ocular symptoms
Vestibular-ocular symptoms include dizziness, poor balance, nausea, and vision changes.
Researchers recommend screening for the specific type of dysfunction, based on which a physician or physical therapist can recommend individualized treatments with vestibular rehabilitation therapy (VRT).
Check out our pages on Vestibular Therapy, Vision Therapy, and Physical Therapy pages, for more information.
Emotional symptoms
A 2019 research study says that the use of cognitive behavioral therapy (CBT) in pediatric cases has been shown to “reduce pain frequency and severity, reduce associated stress, anxiety and depression, improve sleep, and improve functioning across domains, including school and physical activity.”
Other kinds of psychotherapy can also be helpful; see our page on Mental Health for more information
Cognitive symptoms
Researchers suggest that being evaluated by a neuropsychologist with expertise in concussions helps improve the pace of recovery. Only limited evidence was found to support the use of some medications for cognitive symptoms. See our Medication page.
If cognitive symptoms persist, consider Cognitive Rehabilitation Therapy. Read more about post-concussion cognitive dysfunction on our page on Cognitive Dysfunction.
Evidence-based steps for recovery
“Everybody has advice on concussions, but nobody has a plan” - Dr. Susan Klein.
Once a concussion has been diagnosed, and your child has been sent back home, it can be draining and confusing to figure out what to do. It is easy to find advice, but that can be overwhelming when no plan is provided.
All Age Groups
First 12 hours:
If the concussion has caused a headache or other pain:
Avoid any pain medications for the first 4 hours post-injury.
From 4-12 hours after injury, Acetaminophen (Tylenol or other brands) is recommended to help with pain if your child’s healthcare provider approves.
From 4-12 hours, avoid pain meds that thin the blood:
aspirin, ibuprofen (Advil, Motrin), or naproxen (Aleve)
Ibuprofen should never be used in babies under 6 months.
Other tips
Keep your child hydrated
Allow your child to rest
Try to maintain a quiet environment for your child
Maintain supervision
If you observe any irregular breathing or change in skin color, seek immediate medical attention.
If your child cannot be woken up, seek medical attention immediately.
What to do as a parent
If you or another adult (such as a coach) suspects a child has sustained a concussion while participating in sports, remove the child from play and do not let them return to the game. An adult should take the child to see a healthcare provider in a clinic within 24 to 48 hours of the injury unless you observe “Red Flag” signs and symptoms, in which case, take them to the Emergency Department immediately. Your child should not return to sports until cleared by their healthcare provider. If you notice any sudden behavioral or emotional changes in your child after an impact to the head or body, it is possible that your child has sustained a concussion. If you are unsure whether to see a healthcare provider, refer to the “When to see a Healthcare Provider” section.
As a parent, it is your responsibility to report concussions that happen out of school to the child’s school so that they can begin to prepare adequate accommodations. If a concussion occurs at school, it is important that you respond to the school immediately and ensure that the child is assessed as soon as possible by a medical professional.
Once school administration has been informed that the child has sustained a concussion, it may be beneficial to meet with the principal, teachers, learning assistants, nurses, and counselors to figure out a return-to-school plan for the child. It is important to note that all concussions are different, so a return-to-learn should be tailored to each child and may need to be adjusted over time.
According to the latest guidelines, “Complete absence from the school environment for more than one week is generally not recommended.” Please read our Return to School Guidelines for more in-depth information.
You play an important role in following the child’s return to school and making sure that the plan set in place is working. If you notice that your child has been struggling in school, it is important to be proactive with administration and discuss accommodations for the child. Refer to “What to do as a Teacher” for more information about potential accommodations and needs for the child at school.
Refer to our “Return to School” section for more information on your child’s return to learning.
Overparenting
A research article in Child Psychiatry & Human Development was the first to study the associations between overparenting, emotional distress, and recovery time post-concussion. The authors define overparenting as being exceedingly involved or protective and declining to allow children autonomy, possibly leading to deleterious psychosocial outcomes for the child.
While it is important to closely monitor the child’s recovery process and symptoms, any additional stress can lengthen recovery time for concussions in children. We understand that it can be stressful when your child has suffered a concussion, and your instinct may be to stay closely involved with your child’s recovery. However, not being able to return to school, social life, and sports can cause distress. If you appear stressed, your child may become more worried and less focused on recovery. You must be conscientious of the child’s sensitivity and emotional variability when being a caretaker. Talk to your child and try to find the right balance of care for them.
For more information on overparenting, click here.
For more information on what to do as a parent, check out concussion management for children and adolescents, when to go to the emergency room, and CATTonline.
What to do as a teacher
Your role as a school professional in a child’s recovery
A school should always provide adequate supervision of students during physical activities like recess or physical education classes. Making sure that students wear appropriate sporting attire, like closed toed shoes or helmets during certain activities can help protect students.
Every school should have a protocol or procedure for head injuries to determine severity and screen for potential concussion. It is important to develop a proper protocol so that all school professionals will be able to assist and understand when help is needed.
When a student returns to school after a concussion, the school should create a plan with caregivers to establish proper communication and documentation. To learn more, check out the Concussion Awareness Training Tool school professional course.
Education of school professionals on concussions through professional days and information is important for all schools. This could include ensuring that teachers and administrators complete the Concussion Awareness Training Tool school professional course. It is also important to educate students about concussions. Including a session on concussions and head injuries in a physical education course or assembly could help students self-advocate.
How teachers can support return to school
Physical accommodations
Allow more frequent rest breaks
Allow students to wear hats or other protective accessories
Give preferential seating to reduce distractions or bright light
Allow for extra time on assignments and assessments
Provide a reduced distraction testing environment
Plan according to “Return to School” and “Return to Sport” guidelines for physical education and recess
Learn more about concussion in sports and see return-to-learn and return-to-sport guidelines here
Cognitive accommodations
Reduce time at school and workload (prioritize essential work)
Start with half-days if possible for families
Lower academic expectations
Meet for help on assignments and material
Lower homework load
Expect less participation for a short period of time
Avoid overstimulating or noisy environments
Accommodations for reducing stimulation in normally busy environments like lunch in the cafeteria and recess may be necessary
Emotional and behavioral accommodations
Provide opportunities for socialization in comfortable environments
If a child cannot yet return to physical education and cannot participate in physical or overstimulating activities, provide fun alternatives
Allow students to leave class or take breaks when necessary
Keep up communication to help students express themselves
Allow access to counseling
For more information, check out Concussion Awareness Training Tool for school professionals.
Return to school
In the first days after the injury while your child is home resting, communicate with the school to develop a return-to-school plan, even if just an informal one. Consider talking with your child’s teachers, the school nurse, coach, and possibly the school principal or vice-principal.
“The child/adolescent should return to their school environment as soon as they are able to tolerate engaging in cognitive activities without exacerbating their symptoms, even if they are still experiencing symptoms.” Source: PedsConcussion
“Complete absence from the school environment for more than one week is generally not recommended. Children/adolescents should receive temporary academic accommodations (such as modifications to schedule, classroom environment and workload) to support a return to the school environment in some capacity as soon as possible.” Source: PedsConcussion.
Return to School strategy
Scroll below this chart for instructions on how to implement this Return to School strategy
How to use the PedsConcussion Return to School strategy
The instructions and definitions below are from Pedsconcussion.
"Students should begin a gradual increase in their cognitive load with the goal of minimizing time away from the school environment. The return to school should not be restricted if the student is tolerating full days.
Progression through the strategy may be slowed when there is more than a mild and brief symptom
exacerbation**; however, missing more than one week of school is not generally recommended.
Definitions:
*Relative rest: activities of daily living, including walking and other light physical and cognitive activities, are permitted as tolerated.
**Mild exacerbation (worsening) of symptoms: No more than a 2-point increase when compared with the pre-activity value on a 0-10-point symptom severity scale.”
***"Brief" exacerbation of symptoms: Worsening of symptoms for up to 1 hour.
***0-10 point symptom severity scale: Please see the Visual analog scale for an example of a 0-10 symptom severity scale.”
Accommodations in School
Ask the school for return-to-learn accommodations such as:
Return to school part-time
Identify some periods that the student can take off and rest in the nurse's office
Talk with the teacher about scaling back assignments
Ask if your student can do passing periods a bit late or early, to avoid crowded, noisy hallways
Talk with the teacher about postponing tests or setting up special testing accommodations:
Taking the test in a quiet room
Time and a half to take the test
More helpful information
For more about concussion recovery, click here.
If you want to know more about what a school should provide for your child, check out the section “What to do as a Teacher.”
For more information on returning to school, visit returntoschool.org, the Center on Brain Injury Research and Training, Peds Concussion, and SchoolFirst.
Return to sport
We recommend the Return to Activity/Sport Protocol developed by PedsConcussion.
How to Use the Return to Activity/Sports Strategy
When using the Return to Sport strategy in the chart above, follow these instructions from Pedsconcussion. You can use chart called the “Visual Analogue Scale” (below) to help rate your symptoms.
“Begin Step 1 (i.e., relative rest) within 24 hours of injury, with progression through each subsequent step taking a minimum of 24 hours. If more than mild exacerbation (worsening) of symptoms (i.e., more than 2 points on a 0-10 scale***) occurs during Steps 1-3, stop the activity and attempt to exercise the next day.
People experiencing concussion-related symptoms during Steps 4-6 should return to Step 3 to establish full resolution of symptoms with exertion before engaging in at-risk activities. Written determination of medical clearance should be provided before unrestricted Return to Sport as directed by local laws and/or sporting regulations.”
Definitions
“*Relative rest: activities of daily living, including walking and other light physical and cognitive activities, are permitted as tolerated.
**Mild exacerbation (worsening) of symptoms: No more than a 2-point increase when compared with the pre-activity value on a 0-10-point symptom severity scale***. "Brief" exacerbation of symptoms: Worsening of symptoms for up to 1 hour.
***0-10 point symptom severity scale: Please see the Visual analog scale for an example of a 0-10 symptom severity scale.
More Information on Concussion Recovery
For more about concussion recovery for youth, click here.
Reducing concussions in sport
While football, soccer, and hockey may be some of the youth sports most commonly associated with concussions, many sports are underrepresented in research and also have high concussion incidence. Sports such as cheerleading and gymnastics also present high risk for concussion. Take proper precautions in every sporting environment to minimize concussions in sport!
Football
An article published by The Brink, a news source for research at Boston University, titled “CTE risk more than doubles after just three years of playing football,” presents quantitative evidence from the BU CTE Center’s study from 2019. The article presents data from the study, which demonstrates that the odds of CTE in football players increased by 30% for every extra year playing football. This translates to the odds of CTE doubling every 2.6 years of playing football. Interestingly, the strength of correlation remained consistent no matter how many years the individual had played football before. All levels, including youth football, were included in the data. It is important to consider that some research indicates that the earlier your child enters a contact sport, the higher their risk for cognitive issues or even neurodegenerative disease later in life. However, this research is still in relatively early stages, and there are many factors beyond concussive and subconcussive impacts that affect risk level.
We encourage flag football until 14 years old
Many great football players did not play tackle football until 14 years or older
A child’s body is not designed for tackle football
Children are lightweight
Children have larger heads compared to their bodies and relatively lower neck strength
For more information on concussions in football, click here.
Soccer
Given that about 30% of concussions in high school soccer come directly from heading the ball, limiting headers could significantly reduce the risk of concussion in youth soccer players.
U.S. Soccer has implemented concussion guidelines for kids and teens as a way to keep young soccer players safe. These guidelines state that no child 10 and under should be heading the ball during practice or games. The guidelines discourage heading in U12/U13 age groups.
For more information on concussions in soccer, click here.
Hockey
One study found that disallowing “body checking” in youth hockey could prevent half of all concussions at the youth hockey level.
Another study found that practicing bodychecking, and having experience with bodychecking does not decrease rates of injury and actually increases injury rates.
Athletes in general
Dangers of returning to sports too quickly
If children with a concussion go back to activities that include a risk of hitting their head or falling down again too early after a concussion, they can have another concussion.
Having another concussion can lead to worse symptoms that last longer or result in a more severe or fatal brain injury. Second impact syndrome (SIS) is a condition in which an individual sustains a second brain injury during a window of vulnerability following the initial brain injury. This condition is relatively rare, but athletes who sustain a concussion and return to their sport too soon may be at higher risk, as are athletes who remain in the game after a concussion. The syndrome is often fatal but can also lead to severe cognitive disabilities.
For more on concussions in sports, click here.
Mental Health
Concussion Alliance developed the following section on mental health in concussed children. The recommendations are compiled from CATT’s Managing Your Mental Health Symptoms, Concussion Alliance’s blog post on the higher risk for mental health issues in concussed youth, and PedsConcussion's Concussion Recognition, Initial Medical Assessment, Management.
For more, visit our page on Mental Health
Concussion recovery may be understood to be a physically demanding process, but it is equally important to realize that it can also be mentally taxing for your child. Recognizing and managing such mental health concerns is important because psychological well-being plays a critical role in overall health outcomes.
Research has found that concussed youth are more likely to develop mental health issues. (To learn more about one study, visit our blog post on the study here.) This higher risk underscores the need for early intervention and the creation of a secure environment in which your child feels secure to share their thoughts and feelings.
Parents should:
Look for any concerning signs such as behavioral changes in their child
Listen to their child and problem-solve together
Facilitate a support system that allows their child to feel safe and socially connected
Encourage a return to normalcy, as safely as possible
Use clear and concise language that will let the child know what to expect, even if they don’t have all the answers
Stay in communication with their child’s school, coaches, and therapists
Avoiding catastrophizing a concussion
Some strategies to manage mental health challenges during recovery are:
Physical activity, as tolerated: Light aerobic exercise—such as walking or stationary biking—is recommended
Deep breathing exercises: Deep breathing can help to reduce acute stress, anxiousness, or dizziness
Identifying and reducing sources of stress: Help your child to recognize physical, emotional, and behavioral stress responses and to identify their sources
Meditation: Mindful meditation is recommended to aid relaxation and relieve stress
Progressive Muscle Relaxation: PMR involves intentionally tensing and relaxing muscle groups to relieve the tension that can be caused by anxiety and stress
Memory aids: Setting reminders and alarms, or creating a visual calendar to keep track of schedule can ease the stress associated with memory loss
Maintain communication and social life: Help your child to maintain social connections and to combat feelings of social isolation.
Helping your child maintain social connections
When concussions limit children’s opportunities to participate in school and sports, they may feel socially isolated. So, it is imperative that they are connected to a strong support system.
Researchers have found that three main groups that form a self-reinforcing support network for concussed youth are close friends, parents, and youth with a personal history of concussion. Each group assists with different facets of recovery and helps concussed children address common challenges, such as feeling misunderstood or socially isolated, being unable to ask for help, and concerns about returning to school.
Here are some ways you can support your child:
Closely communicate with your child and help them stay connected to their close friends or other children who have suffered concussions.
Beyond the initial period of cognitive and physical rest (24-48 hours after injury), encourage your child to participate in rewarding social activities, modified as needed to avoid the risk of worsening symptoms or re-injury.
Spend time with your child doing activities that will not worsen their symptoms, like going on walks, coloring, painting, and safe cooking or baking steps such as mixing or decorating.
Types of social connections a parent can encourage for their child
This infographic is provided by You-Can resources and Dr. Nick Reed at Oak Concussion Lab.
How parents can best advocate with providers
Parents can best advocate for their children by:
Speaking up and communicating with your provider if you don’t think your child is receiving appropriate medical care. You can ask for a referral to a concussion or outpatient rehabilitation clinic.
Asking for support and updates from your child’s teachers and relaying appropriate information to (and from) your child’s doctor.
Being patient and remembering that recovery is a process, and sometimes a slow one. Help your child to stick to their recovery plan and let them know that their brain is healing.
Joining a parent support group or organization. Seek support from other parents in your community who have experienced a child sustaining a concussion. You will likely be surprised at how common this injury is.
Peer Support
Taking care of your child during concussion recovery can be confusing and isolating. For emotional support, we recommend you look at our peer support resource. We always recommend that you get advice from experts rather than these forums.