Neurodegenerative Disease
Researchers continue to examine links between brain injuries and neurodegenerative diseases. The four primary neurodegenerative diseases which may be linked to brain injury are Amyotrophic Lateral Sclerosis (ALS), Parkinson’s disease, Alzheimer’s disease, and Chronic Traumatic Encephalopathy (CTE).
Table of Contents
General information: concussions, subconcussive impacts, and neurodegenerative disease
Chronic Traumatic Encephalopathy (CTE)
General information: concussions, subconcussive impacts, and neurodegenerative disease
Researchers are still examining links between concussions, repetitive subconcussive impacts, and neurodegenerative disease.
Persistent post-concussive symptoms should not be equated with neurodegenerative disease.
There are four primary neurodegenerative diseases thought to be linked to concussions and repetitive subconcussive impacts: Chronic Traumatic Encephalopathy (CTE), Alzheimer’s Disease, Parkinson’s Disease, and Amyotrophic Lateral Sclerosis (ALS).
No cures for these diseases have been discovered, but treatment options to alleviate symptoms are available.
Researchers are still examining how these diseases spread in the brain and potential methods to delay progression.
The mechanisms of these neurodegenerative diseases are different. CTE, Alzheimer’s, and dementia are associated with the buildup of harmful proteins in the brain. Parkinson’s is associated with degeneration of a specific brain region called the basal ganglia. ALS is associated with the destruction of motor neurons throughout the body.
Research on neurodegenerative disease
Researchers are working to uncover the origins and possible treatments of these neurodegenerative diseases. The four main neurodegenerative diseases listed above have different causes and symptoms and should not be lumped together. The current scientific consensus is that neurodegenerative disease is likely associated with repeated exposure to concussions and subconcussive impacts. For example, in one study examining 7676 former Scottish professional soccer players, it was determined that these players were three times more likely to die from neurodegenerative disease than the general public. The primary cause of death was neurodegenerative disease for 1.7% of the players compared to 0.5% of the general public.
While the risks of neurodegenerative disease after concussions or subconcussive impacts are important to note, most people who experience a brain injury will not develop a neurodegenerative disease. Consult a healthcare professional if you are concerned about your risk of developing a neurodegenerative disease.
Persistent post-concussive symptoms and treatment
There are 3.8 million concussions diagnosed annually in America from sports alone; up to one-third develop persistent post-concussive symptoms. Persistent post-concussive symptoms are not the same as neurodegenerative diseases and are more common than any of the four major diseases listed on this page. For information on persistent post-concussive symptoms, visit our webpage.
Concussion Alliance strongly encourages seeking care when experiencing these symptoms. See our guidelines for recovery and treatment options here.
Evidence of inadequate care is not limited to the recognition of PPCS, but also the recognition of concussions in the first place. In a study that examined concussion evaluations in the 2018 World Cup, researchers found that FIFA’s concussion evaluation protocol was not followed in 63% of potential concussions.
Within the Concussion Alliance community, two of our members have experienced insufficient evaluations of their concussions. For one member, her headaches were initially misattributed to an electrolyte imbalance because her physician was skeptical that opening a door in her face could have caused a concussion. For the other member, his neurologist prescribed an MRI, which cannot detect a concussion. Since the MRI did not show any abnormalities, the neurologist thought that he was just in a “pain loop,” and prescribed medication. It took several years before this member finally met a physician that could accurately explain his symptoms.
Chronic Traumatic Encephalopathy (CTE)
CTE is thought to be associated with multiple concussions and repetitive subconcussive impacts.
CTE is thought to be caused by the buildup and spread of harmful proteins in the brain.
Researchers are still examining links between multiple concussions, repetitive subconcussive impacts, and CTE.
Currently, CTE can only be diagnosed after death, but researchers are working on methods to develop diagnoses in living patients.
Experts say CTE symptoms and signs can develop over years and decades.
There is no cure, but prevention is possible through education on concussion and subconcussive impact prevention.
CTE is NOT an inevitable side effect of playing sports such as American football, soccer, or boxing.
Symptoms of CTE
According to the Mayo Clinic, these general changes can be observed in those who experience CTE:
Mood disorders
Depression, apathy, emotional instability, substance misuse, and suicidal thoughts or behavior.
Cognition
Difficulty thinking (cognitive impairment), memory loss, problems with planning and executing tasks (executive function).
Motor
Parkinsonism and motor neuron disease.
Behavioral
Impulsive behavior and aggression.
Stages of CTE
Recent research has indicated that CTE is progressive (its severity increases with time). CTE develops over a course of four stages. According to an article published in Brain: A Journal of Neurology, "Symptoms in stage I chronic traumatic encephalopathy included headache and loss of attention and concentration. Additional symptoms in stage II included depression, explosivity [episodes of uncharacteristic rage] and short-term memory loss. In stage III, executive dysfunction and cognitive impairment were found, and in stage IV, dementia, word-finding difficulty and aggression were characteristic."
When to see a doctor:
Suicidal thoughts. Research shows that people with CTE could be at higher risk of suicide. If you have thoughts of hurting yourself you can call 911, your local emergency number, or the National Suicide Prevention Lifeline at 800-273-TALK (800-273-8255).
Memory problems. See your doctor if you have concerns about your memory, behavior, or cognitive abilities.
Personality or mood changes. See your doctor if depression, anxiety, aggression, or impulsivity occur.
Visit the Mayo Clinic’s page on CTE for more information.
Associations between repetitive brain injuries and CTE
Chronic Traumatic Encephalopathy (CTE) is thought to be caused by repetitive brain injury. It can develop over the course of years and even decades. CTE is currently only diagnosable after death through brain examination. However, researchers aim to establish a system to diagnose CTE in live patients. Scientists are also researching ways to properly diagnose Traumatic Encephalopathy Syndrome (TES), a disorder associated with CTE. According to the Boston University Brain Bank, "Diagnosed concussions are not reliable indicators of CTE," and around 20% of people diagnosed with CTE had never been diagnosed with a concussion.
CTE is thought to spread due to malfunctioning proteins in the brain. One specific protein known as tau is commonly associated with CTE. Healthy and functional neural circuits become damaged through the reproduction and spread of tau in the brain. Recent research has indicated that CTE is progressive (its severity increases with time).
CTE develops over a course of four stages. According to an article published in Brain: A Journal of Neurology, "Symptoms in stage I chronic traumatic encephalopathy included headache and loss of attention and concentration. Additional symptoms in stage II included depression, explosivity [episodes of uncharacteristic rage] and short-term memory loss. In stage III, executive dysfunction and cognitive impairment were found, and in stage IV, dementia, word-finding difficulty and aggression were characteristic."
Organizations such as the Boston University Brain Bank aim to better understand CTE and the mechanisms underlying it by studying the nervous systems of deceased American football players and other athletes. Therapy options for CTE, such as light therapy, are in very early stages of development.
CTE is not the same as persistent post-concussive symptoms, and most people with persistent post-concussive symptoms will not have CTE. Therefore, Concussion Alliance strongly recommends that those who experience persistent symptoms pursue treatment options. To learn more, visit our page on persistent post-concussive symptoms.
Further resources
We highly recommend this article by Elizabeth Sandel, MD, Repetitive Brain Trauma and Chronic Traumatic Encephalopathy (CTE).
For information on the mechanisms of and treatment for CTE, visit Concussion Legacy Foundation. Concussion Alliance recommends this expert talk discussing the history of CTE and common CTE misconceptions by Dr. Willie Stewart.
Dementia and Alzheimer's
Age as well as the number and severity of a person's brain injuries may be risk factors that increase the likelihood of developing dementia and Alzheimer's.
Researchers are studying possible interactions between genetic risk factors, brain injury and Alzheimer's although no consensus exists right now.
Many studies suggest an association between repeated exposure to concussions or subconcussive impacts and dementia and Alzheimer's.
It is important to note that most people who sustain brain injuries such as concussions never develop Alzheimer's disease or later dementia. More research is needed to understand the link between brain injury and dementia and Alzheimer's.
Background on dementia
The risk of developing dementia and Alzheimer's is believed to increase after repeated exposure to concussions or subconcussive impacts. While there is evidence associating brain injury with dementia and Alzheimer's, it is important to note that most people who experience a concussion or subconcussive impact will not experience dementia or Alzheimer's.
Dementia and Alzheimer’s risk factors
Risk factors separate from the injury itself, such as age, may affect the likelihood of developing dementia and Alzheimer's. The scientific consensus is that as age increases, so does the risk of developing dementia and Alzheimer's, especially when taking into account brain injury. Certain genes may serve as risk factors, as well.
There have been increasing calls to investigate connections between brain injuries and dementia. Many important studies have been released in recent years providing evidence for the association between brain injury and the development of dementia. Findings from one study that surveyed over 300,000 veterans suggest that the risk of developing dementia increases from 2.6% to 6.1% in veterans after a mild TBI with no loss of consciousness and can increase according to the severity of the injury.
Another study, in 2021, found that the risk of former professional Scottish football (soccer) players developing dementia increased with the length of their career and the positions in which they played - some of which involved high-force heading. This article in The Herald helps explain the study. A 2019 study by the same team found that footballers had 3.45 times the rate of “Mortality with neurodegenerative disease listed as the primary cause,” compared to a control population.
Further questions and treatment
The Mayo Clinic's website has up-to-date information on dementia treatment. For Alzheimer’s clinical practice guidelines, visit Alzheimer's Association and the American Academy of Family Physicians. For more information on the mechanisms of dementia and Alzheimer’s spread, visit NIH.
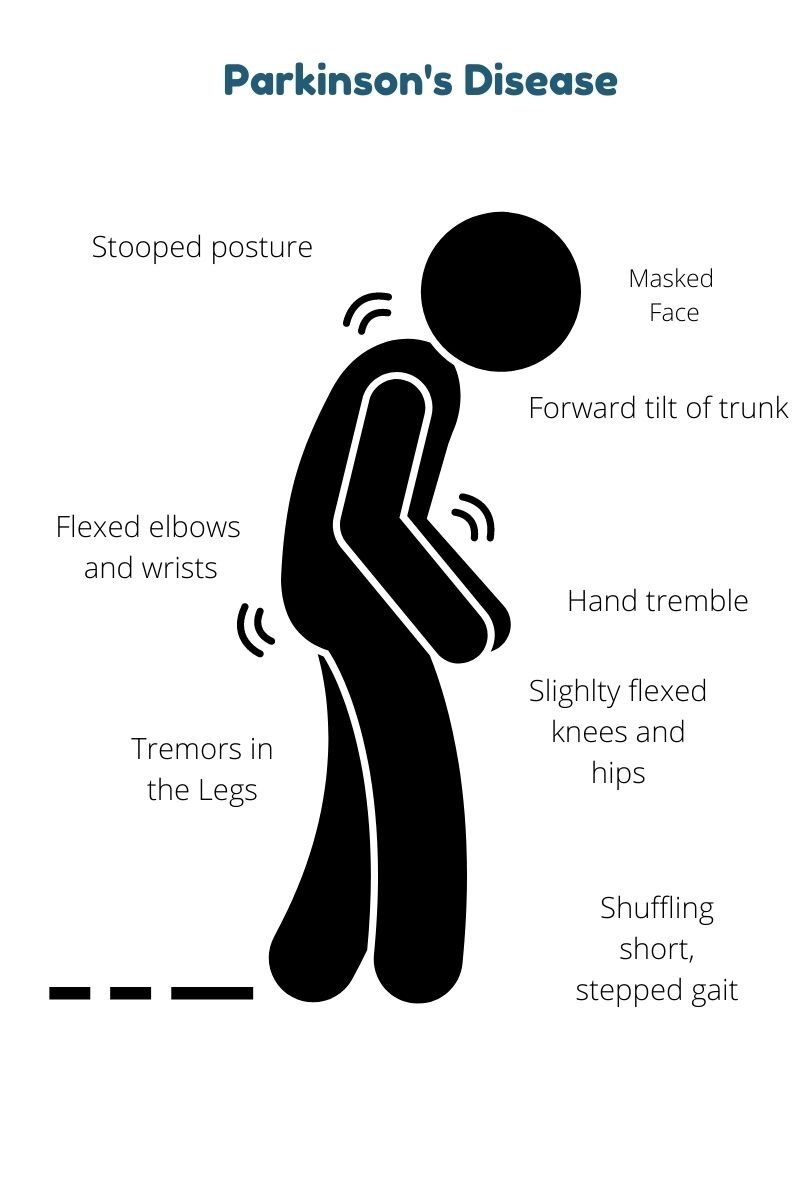
Parkinson’s disease (PD)
Parkinson's disease (PD) is the second most common neurodegenerative disease behind Alzheimer's, with 1 million Americans currently living with this condition.
There is an increased risk of Parkinson's after sustaining a concussion. The lifetime risk of developing Parkinson's disease for the average American is 6.7%.
Background about Parkinson’s disease
According to the National Institute on Aging (NIA), "Parkinson's disease is a brain disorder that leads to shaking, stiffness, and difficulty with walking, balance, and coordination." Men are 1.5 times more likely to develop Parkinson's than women.
Parkinson's disease starts around age 60 for most people, but about 5-10% of cases are early-onset, where patients develop symptoms around age 50. Early-onset Parkinson's is usually inherited. There is no cure for Parkinson's disease, but medications and therapy can control symptoms, often dramatically. For more information, visit the UK NHS website.
Parkinson's disease symptoms result when "nerve cells in the basal ganglia (an area of the brain that controls movement) become impaired and die. Normally, these nerve cells, or neurons, produce an important brain chemical known as dopamine." When these cells die, it inhibits the brain's ability to produce dopamine—this inability to produce dopamine is a hallmark of Parkinson's disease. Researchers are still unsure of what causes impairment or death of these cells.
Research about concussions and Parkinson’s disease
A nationwide study performed by researchers at UCSF investigated the association between traumatic brain injury (TBI) and the onset of Parkinson's disease in veterans. The study found that veterans who sustained a concussion had a 56% increased risk for Parkinson's disease. They also found that the risk was higher (83%) among veterans with moderate-to-severe TBI.
Veterans with any severity of TBI were diagnosed with Parkinson's disease an average of two years earlier than veterans who had not sustained a TBI. Interestingly, because "the majority of TBIs sustained by military veterans occur during civilian life either before or after military service, the results of this study may additionally have important implications for civilian and athlete populations."
A study published in the journal Family Medicine and Community Health found that, regardless of socioeconomic status or residence, having one concussion led to a 57% increase in patients' likelihood of developing Parkinson's disease. They also found that sustaining multiple concussions further increased the risk of developing Parkinson's disease.
Treatment options and learning more
If you have questions about treatment options or Parkinson's disease in general, please visit the Parkinson's Foundation website or the NIH website on Parkinson's.
Amyotrophic Lateral Sclerosis (ALS)
There are two types of ALS: familial ALS and sporadic ALS.
In the United States, less than 0.1% of the population lives with ALS.
There is no cure for ALS.
The association between concussions, subconcussive impacts, and ALS is disputed and needs further research.
NFL athletes are four times as likely to develop ALS than the general US population.
Research investigating the association between ALS and concussions
Although several studies have found an association between traumatic brain injury (TBI) and ALS, there is no consensus on whether TBI is an ALS risk factor. A population-based study published in 2017 found that a history of 2 + TBI was associated with an almost three-fold increased risk of ALS. The risk was almost two-fold more when the trauma occurred at age 35-54. However, many of the TBIs in this study were moderate to severe TBI, resulting in the patient having a disability. Concussions do not fall under the category of moderate or severe TBI.
Additionally, a 2019 review article published in the Journal of Neurophysiology said that concussions "can cause ALS in a subset of susceptible patients, based on a history of repetitive mild TBI and genetic predisposition." Finally, a study published in the Journal of the American Medical Association (JAMA) in 2021 found that NFL players have a four-fold increased rate of developing and dying from ALS. However, there was no link to specific types of impacts that led to ALS, just the length of the NFL career, preventing generalization to the U.S. population. Due to how recent this study is, Concussion Alliance is unsure how this study will shift the understanding surrounding ALS, subconcussive impacts, and concussions.
Background Information
ALS is an always fatal neurodegenerative disease in which the person's brain loses connection with the muscles. The nerve cell with sclerosis in the picture below is an example of a nerve cell that cannot contract muscles. People with ALS will lose their ability to walk, talk, eat, and eventually breathe. There is currently no cure for ALS. According to Johns Hopkins Medicine estimates, 30,000 Americans are now living with ALS. This means that on average, for every 100,000 people living in the United States, just over five people are living with ALS.
ALS can affect anyone at any time but most often presents in people from ages 40 to 70.
There are two different types of ALS, sporadic and familial. Sporadic, an occurrence without a family history, is the most common form of the disease in the U.S. and accounts for 90 to 95 percent of all cases. Familial ALS (FALS), an inherited disease, accounts for 5 to 10 percent of all cases in the U.S.
ALS manifests differently than CTE: In ALS, people typically have a gradual progression of weakness, and in CTE, they frequently have signs of dementia, Parkinson's-like syndrome, and behavioral problems.
Treatment options and further steps
For treatment options and to learn more about ALS, please visit ALS.org or OHSU's website on ALS.































The National Institutes of Health (NIH) recently acknowledged that there is a causal link between repeated blows to the head and chronic traumatic encephalopathy (CTE).