Partner-Inflicted Brain Injuries
A step-by-step guide to recognizing, understanding, and advocating on behalf of those affected by intimate partner violence (IPV) related traumatic brain injuries.
IF YOU BELIEVE THAT YOURSELF OR SOMEONE YOU KNOW IS EXPERIENCING INTIMATE PARTER VIOLENCE, DO NOT HESITATE TO FIND IMMEDIATE SUPPORT BY CONTACTING THE RESOURCES PROVIDED BELOW:
Chat: Open this link
Phone: 1.800.799.SAFE (7233)
Text: Text “START” to 88788
More resources:
Domestic Violence Shelters in the United States
Love is Respect: National Teen Dating Abuse Hotline
Rape, Abuse & Incest National Network's (RAINN) National Sexual Assault Hotline
Table of Contents:
Connecting Intimate Partner Violence and Brain Injuries
Defining Brain Injury | Intimate Partner Violence
Difficulty Diagnosing Brain Injury in General | Difficulty Diagnosing Brain Injury in IPV |
Screening for an IPV-related Brain Injury
Long Term Consequences of IPV-Related Brain Injury
Women as a Research Population | Future areas of research
Stigma in IPV Survivors | Supporting Survivors as a Friend or Family Member
Advocating for yourself in interaction with healthcare professionals
Connecting Partner Violence and Brain Injuries
“We have overlooked this pandemic for too long: traumatic brain injuries in women subjected to intimate partner violence”
- Eve Valera, PhD
What is a Brain Injury?
According to the Brain Injury Association of America:
Brain injury occurs when brain function is altered by an external force. This happens when something strikes the head or when the head hits something as the result of a fall, motor vehicle accident, assault, and more. There are many different causes of TBI and several different types.
This also encompasses “damage to the brain as a result of internal factors, such as a lack of oxygen, exposure to toxins, and pressure from a tumor.”
Brain injuries can include loss of consciousness but do not have to. It does not have to be a direct hit to the head
What is intimate partner violence (IPV)?
Intimate Partner Violence (IPV): violence perpetrated by a current or former romantic or sexual partner that causes physical, sexual or psychological harm.
NOTE: IPV is a subcategory of domestic violence. It is important to recognize that brain injuries can occur in other realms of domestic violence, such as injuries inflicted by parents on children (child abuse) and other family members on elders (elder abuse). While these types of domestic violence-related brain injuries will not be discussed on this page, you can learn more about these populations on our website.
Here are some quick facts to illustrate the broad scope of IPV:
IPV is the leading cause of homicide for women globally.
IPV is the most common form of violence against women worldwide.
IPV has been shown to traverse all socioeconomic boundaries.
Diagnosing the Injury
“Women don’t know they are sustaining these brain injuries…they go unnoticed and unacknowledged, but they may have long-lasting effects.”
Brain injury is often referred to as a ‘hidden epidemic’; Brain injury in those experiencing IPV is prevalent, yet many cases are misdiagnosed, undiagnosed, and untreated.
As a result, women with IPV are often unaware they are experiencing brain injury.
Why is this?
Difficulty Diagnosing Brain Injury in General
Brains of those with more mild forms of brain injury will appear normal on typical MRI or CT scans - these scans only show skull fractures or brain bleeds, more severe forms of brain injury
Even then, CT scans or MRIs are not often ordered due to accessibility or affordability
In summary:
Brain injury is often an invisible injury
Diagnosis relies primarily on the patient’s signs and symptoms
Because of this…
Brain injury is easily misunderstood and difficult to treat by healthcare providers
Symptoms look different for everyone so it is important to have individualized treatment and a comprehensive patient history taken!
Difficulty diagnosing brain injury for IPV
In addition to the general difficulty in diagnosing brain injury, there are problems associated specifically with IPV:
Symptomatic overlap
Many of the symptoms of brain injury closely resemble the physical and psychological effects of intimate partner violence.
Venn diagram showing overlap between symptoms of IPV and TBIs. Symptoms were obtained via a cross-reference comparison of symptoms listed for “domestic violence” or “concussions” on the PsychCentral and CDC websites, respectively.
Limited knowledge from domestic violence shelter staff on brain injury
The stigma surrounding IPV, both internalized and from societal stereotyping and treatment, can make survivors less likely to look for medical care immediately after their injury or fully disclose what caused their injuries
Due to the combination of factors including difficulty diagnosing brain injury generally and for IPV, it is easy to mistake typical signs of a traumatic brain injury for symptoms as a result of intimate partner violence, PTSD, or other conditions, especially as both often occur simultaneously. It is essential to use proper screening practices to ensure accurate diagnosis and appropriate care.
Without proper diagnosis, women may be left feeling as though the issues are their fault or just "in their head," but this is not the case. Receiving a diagnosis is often the crucial first step toward recovery or adapting to a new way of life.
“But it was 15 years when I started noticing symptoms, but I didn't know what those symptoms were related to. And it wasn't until I spoke with Dr. Valera in 2016, 2017, when I finally had answers. And having an answer to what was going on with me was such a relief. And it also allowed me to realize that what happened to me was not a shameful thing. The shame did not belong on me. The shame belonged on him.” - Freya Doe, a domestic violence survivor
Screening for an IPV-related Brain Injury
Disclaimer: There are many different screening tools that are currently being both recommended and used by various state-wide organizations. In six states, there are conflicting recommendations for different screening tools from different state organizations as of 2020.
In addition, these screening tools alone should not indicate whether a brain injury is or is not present, it only assesses potential of a brain injury. Instead, for maximum effectiveness, these tools should be used in combination with clinical assessment.
There is no universally accepted screening tool for brain injury but here are several listed below commonly used in research or treatment of IPV related brain injuries:
HELPS Brain Injury Screening Tool
The HELPS Brain injury screening tool was first developed M. Picard, D. Scarisbrick, R. Paluck, in 1991 at the International Center for the Disabled. It now has been widely adopted to assess brain injury in many settings.
This version of the HELPS screening tool has been adapted by the SOAR Project (Supporting Survivor of Abuse or Brain Injury Through Research)
Ohio State University TBI Screening Tool (OSU TBI-ID)
This tool assesses TBI over a lifetime through a 3-5 minute structured interview, making it extremely helpful for IPV survivors. It is widely used for both research and clinical purposes.
Brain Injury Screening Questionnaire (BISQ)
This tool, developed by the Icahn School of Medicine at Mount Sinai, screens for a lifetime of TBIs. It is used in many diverse settings and evaluates four domains: attention and memory; depression, anxiety, and mood; aggression and impulsivity; and physical symptoms. The BISQ may be completed via interview or self-administration.
Long Term Consequences of IPV-related Brain Injury
IPV is unique in that brain injuries are repeatedly sustained often without being recognized, aggravating symptoms and increasing risk
Each subsequent concussion increases risk for another concussion
This is especially dangerous in the context of second impact syndrome, which is a rare but dangerous event that can occur when another brain injury happens during a small window of vulnerability after a previous brain injury. This can cause severe swelling and bleeding in the brain and death.
Brain injuries also can lead to long-term impacts after the initial injury, resulting in symptoms such as…
Decreased cognitive functioning
Mood changes
Sleep difficulties
Somatic issues such as headaches, nausea, and more
These symptoms are often compounded by PTSD and other conditions associated with experiencing IPV.
Did you know?
Many treatments exist to treat symptoms of brain injury and many people are able to recover or make significant progress. Learn about treatments and self-care options on our Overview of Treatments and Self-Care page.
There are also many resources to receive a diagnosis or treatment for a brain injury for survivors of IPV.
For primary or preventative healthcare services:
Click here to use the Find a Health Center tool.
To find knowledgable and qualified providers for concussion care:
Visit our Find Providers page.
For underserved populations or uninsured populations:
Health Resources and Services Administration (HRSA) funded health centers are specifically designed to serve medically underserved communities. These centers provide comprehensive healthcare services regardless of patients' ability to pay, ensuring access to high-quality care for those who may not have other options.
Understanding the Research
Women & Girls as a Research Population
“Women and girls suffer silently or scream for help where there seems to be none for too long - they are our mothers, daughters, granddaughters, sisters, nieces, and friends”
— Marilyn Spivack, President of the National Head Injury Foundation, Emeritus
Historically, there has been a lack of research on TBI in women compared to men. This is concerning because growing evidence shows that the effects of TBI differ between men and women, potentially requiring different treatment approaches for each. Given the limited research on women, it is even more critical to expand studies in this area, particularly in light of the observed sex differences in TBI between women and men, especially in the context of IPV. Unfortunately, this research is often underfunded and overshadowed by the focus on male sports.
A majority of research has found women differ from men regarding brain injury in…
Women Differ in Incidence
Many studies have found female athletes are more likely to sustain a concussion than their male counterparts. For example, a study conducted at the University of North Carolina at Chapel Hill found that girls who play high school soccer almost sustain the same rate of concussions as a male high school football player. In addition, in sex comparable sports the overall concussion rate was higher in girls than in boys.
Women Differ in Symptomatology
Studies indicate women are at a higher risk for post concussion symptoms and report a greater number of symptoms in comparison to men
Research has found women experience more severe post concussion symptoms and perform worse in neurocognitive testing following a brain injury.
Another study found female TBI patients between the ages of 0-18 were 3.2x more likely to develop a hormonal disorder, which can stunt growth and lead to cognitive deficits.
Women Differ in Recovery
Dr. John Leddy and Dr. Barry Willer of the University of Buffalo found that while women presented with significantly more initial symptoms than men, these symptoms were significantly reduced when women were prescribed a light aerobic exercise routine instead of prolonged rest. This demonstrates how women may be more susceptible to symptom increases from strict rest than men.
Women Differ in Structure
Dr. Doug Smith of the University of Pennsylvania conducted a groundbreaking study using imaging technology on the brains of both female and male rats and humans. He discovered that female axons—nerve fibers that connect neurons and enable communication—are smaller and have fewer microtubules, which are the "train tracks" that transport molecules along the axon. This difference suggests that female axons are more fragile and more likely to break due to the blunt force of brain injury.
Figure from the landmark study by Dr. Doug Smith of the University of Pennsylvania Medical School.
Studies have also suggested that female athletes may have a lower biomechanical threshold for concussions, potentially due to shorter neck dimensions, less head mass, and a narrower neck girth. These factors could increase the risk of greater head and neck acceleration in females than in males during impacts. “Wilcox et al. found that concussive impacts in women’s hockey generated a mean PLA of 43g ± 15g. This is significantly lower than the PLA associated with concussive impacts in male collegiate football players (range, 60.51-168.71g.”
A Stanford study found that women had significantly more cortical thinning (thinning of the cerebral cortex) than men after sustaining a TBI. While cortical thinning occurs naturally with aging or neurodegenerative disorders, it has been found to be accelerated by TBI, leading to potential impairments in emotional regulation or decision making.
Hormones and phases in the menstrual cycle can influence the severity and outcomes of symptoms following a brain injury.
Women Differ in Reporting
Women are more likely to report brain injury to an authoritative figure more often than men when both had similar levels of knowledge around sports-related concussions. This difference may be due to societal factors such as the culture within the male sports environment where masculinity and ‘playing through pain’ is often encouraged.
However, it's important to acknowledge the nuance in this research. While many studies have identified sex-based differences in traumatic brain injuries, other studies have yielded different results. This highlights the need to consider various factors, such as age or more when conducting research in this area.
Future areas of research
Understanding Sex Differences in Post-Concussion Symptoms: Investigating whether the differences in post-concussion symptoms between women and men are due to societal behavior, biology, or a combination of both, to improve treatment approaches.
Concussion Management Across Diverse Groups: Tailoring concussion management strategies to address the unique needs of various groups of women, including veterans, students returning to school at all ages, IPV survivors, homeless populations, transgender individuals, and more. Each group faces distinct challenges, making it crucial to develop specific approaches that ensure effective and equitable care.
Education for Healthcare Providers: Enhancing the education of healthcare providers to improve their ability to recognize, treat, and manage concussions effectively.
Research into Biomarkers: Expanding research into biomarkers to better diagnose and treat concussions.
For IPV survivors specifically:
Obtain estimates of IPV related brain injury and/or strangulation in the general population
Assess the combined effects of strangulation and brain injury when they occur simultaneously.
Examine the effects of brain injury on cognitive, psychological, and social functioning on IPV survivors.
Develop biomarkers for diagnosis, prognosis, and historical assessment specific to IPV related brain injury.
Conduct research to understand the long-term effects of IPV-related brain injuries, including the potential for chronic neurological disorders or dementia.
At-Risk Groups
Return to hotline resources at the top of the page
Minority Women
Racial minorities have greater difficulty reintegrating into their communities following a TBI. This includes resuming household duties, workplace responsibilities, and social activities.
Hispanic and Black participants were found to have many misconceptions regarding TBIs, specifically about symptomology and recovery.
Promisingly, Dr. Pappadis found that these misconceptions could be corrected via educational interventions.
In the context of IPV, many minority women have misconceptions that may further impact their ability to seek treatment. In addition, minority women might have more trouble leaving violent IPV situations due to difficulties resuming household/workplace duties.
Mothers
“Intimate partner violence is often a life-threatening event to both the mother and the fetus.”
Dr. Jay G. Silverman from Harvard School of Public Health found that women experiencing IPV before and during pregnancy have a risk of poor maternal and infant health outcomes. Mothers are at increased risk for high blood pressure, vaginal bleeding, severe nausea, vomiting, and kidney infection. Hospital visits are more frequent due to morbidity and the infants delivered are at higher risk of being preterm, low in birth weight, and needing intensive care unit care.
However, even after delivery, these women can experience erratic behavior from their repetitive TBIs that serve as additional hardships towards readjusting to their former lifestyle. These hardships become particularly salient for mothers who not only have to care for themselves but also their children. In addition, the presence of children can increase a woman's inability to escape from an abusive relationship.
Veterans
There are over 2 million female veterans in the United States. This group of women displays a 1.6 times higher rate of experiencing IPV than their non-military peers.
Many studies in the field have been lead by Dr. Katherine Iverson and Dr. Terri Pogoda from Boston University. So far, they have found that female veterans with an IPV-related TBI history had significantly higher levels of depression and PTSD, greater utilization of Veteran’s Affairs (VA) healthcare, and poorer perceived physical health than women who experienced IPV to the head region, but had no diagnosed TBI.
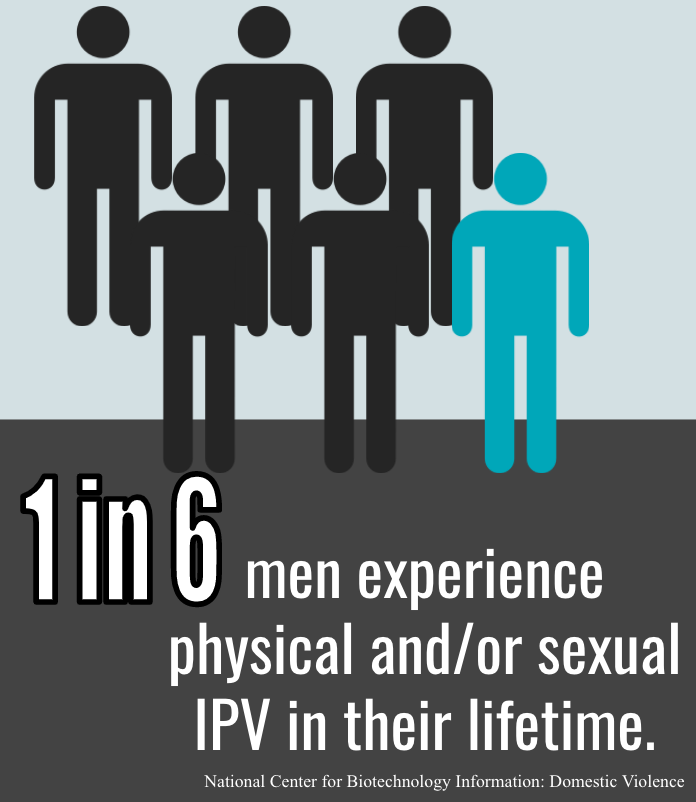
What about IPV-Related Brain Injury in Men?
Great Question!
Unfortunately, research on this topic is even more limited than IPV related brain injury in women.
Here is what we do know:
Estimates show that about 4% of men in the United States, or 2.5 million men, are victims of severe IPV from their partners each year.
These male victims display higher levels of stress, depression, PTSD, and substance abuse.
The criminal justice system in America often does not support men as victims in these situations.
At this time, the prevalence of traumatic brain injuries from IPV in male populations has yet to be formally investigated. However, it certainly should be as these men are a distinct population that face their own unique challenges towards receiving adequate treatment such as…
Many men hesitate to seek treatment due to fears that they will be ridiculed or embarrassed.
Male victims attest that the police will fail to respond, take a report, and in some cases, will even arrest the man as the violent perpetrator despite there being no evidence of injury to the female partner.
Domestic violence support resources such as hotlines will assume the man is the perpetrator and even direct them to batterers’ programs.
These internal and external barriers that male victims of partner-inflicted TBIs face can increase their difficulty in finding the treatment and resources that they need.
How to Support Survivors
Stigma in IPV survivors
Having conversations with IPV survivors about their situation can be hard even as a friend or a family member. There are many stigmas that prevent survivors from opening up such as feeling embarrassed of their situation, uncomfortable of sharing, and scared of repercussions especially if the information gets leaked. One way the National Domestic Violence Hotline offers as a support is to acknowledge the difficulty and the fear of the survivors' situations to create a destigmatized space for conversation. As a friend or family member, we can reassure survivors by saying the abuse is not their fault, they are not alone, and there is support available including from yourself.
Supporting Survivors as a Friend or Family Member
Emotional Support
The experience of the relationship could provoke complex emotions for IPV survivors. To help process these emotions and navigate the next steps, the following advice from the National Domestic Violence Hotline are ways to provide emotional support.
Acknowledge that their situation is difficult, scary, and brave of them to regain control from.
Be supportive of them in their decisions and choices by not judging, criticizing, or guilting survivors.
Remember that you cannot “rescue them,” their decisions are about their lives and up to the survivors to make.
Not speaking poorly of the survivor’s partner.
Help them create a safety plan.
Offer to go with them to any service provider or legal setting for moral support.
Material Support
Some survivors may be in a situation where they are financially dependent on their partner or lack access to material resources. As an immediate support, the National Domestic Violence Hotline provides advice with the following on ways to help with their material needs.
Help survivors identify a support network to assist with physical needs like housing, food, healthcare, mobility, etc.
Assist in storing important documents or creating a “to-go bag” in case of an emergency situation.
Encourage survivors to talk to people who can provide professional help and guidance.
If the survivor gives you permission, help document instances of injuries in their life, including pictures, exact transcripts of interactions, and notes on dates that incidents occur.
Invite survivors to participate in activities outside of their relationship with friends and family.
Not posting information about survivors on social media that could identify them or show where they spend time.
Advocating for Yourself in Interaction with Healthcare Professionals
To receive proper diagnosis and care, it is important to be honest about any IPV experiences to your healthcare provider. Most doctor offices will listen to a patient's decision on allowing their partner to be present during visits. If requesting privacy might provoke danger after the appointment, the National Domestic Violence Hotline suggests contacting your provider beforehand to ask if they could tell your partner about speaking to the patient alone.
Always trust your instincts and judgment that ensure your safety.
In some cases, IPV survivors are faced with invalidation during their interaction with healthcare providers. According to a systematic review by Heron & Eisma, barriers to disclosing violence to healthcare service includes the negative evaluation from healthcare providers by being unsympathetic, disinterested, and not listening. The lack of a positive relationship with the provider leads to a lack of trust, decreasing the time spent in each visit, and low continuity in attending appointments. The DomesticShelters.org provides the following advice for survivors to advocate for themselves.
Explain your symptoms factually, clearly, and quickly. The National Domestic Violence Hotline recommends writing down what you would like to discuss with the provider to avoid missing important information.
Ask them for a referral to a specialist, another physician in the practice, and different screening options.
Ask what to do if the symptoms get worse. What if the symptoms aren’t just anxiety or related to PMS? What happens if they don’t go away or escalate in severity?
Ask what else the symptoms could be because it could open up a broader conversation that could highlight potential concerns that may have been overlooked.
What a good screening looks like
Valid screening tools should:
Include open-ended questions that allow the participant to explain their story.
Not include any invasive, probing questions that can trigger historic brain trauma.
Recognize that consciousness is a continuum (i.e. some patients will experience a loss of consciousness while others will only have a partial loss of memory).
Be administered via paper and pencil so as not to trigger light sensitivity and related symptoms of people experiencing a brain injury.
Be conducted in a safe environment without any partners or other family members present.
Provide safety-planning and connect women with desired resources should they screen positive for an IPV-related TBI.
Introducing Supportive Organizations
Return to hotline resources at the top of the page
Fortunately, there are lots of great non-profit organizations that are working to raise awareness and support for victims of parter-inflicted brain injuries. We will highlight a few of these organizations and the resources they offer below:
-
Abused and Brain Injured strives to bridge the educational gap between intimate partner violence and brain injury. They provide toolkits with resources, research, and practice recommendations to assist patients and providers in accessing the most up-to-date information.
-
Created in 2012, the Domestic Violence Brain Injury Program was one of the first of its kind in the United States to identify and treat brain injuries related to intimate partner violence. This is done in a few ways…
Free clinical care; regardless of insurance, patients will be evaluated by a specialist and connected with a social worker to assist in navigating the health care system
Cognitive retraining classes held at partner shelters
Educating providers and the community on brain injuries and the identification of symptoms
Partnering with local organizations to raise awareness
Clinical research pertaining to improved treatments and the potential long-term outcomes of a brain injury
-
ODVN aims to support and strengthen Ohio’s response to domestic violence through direct survivor support, training, public awareness, and technical assistance and to promote social change through public policy implementation.
Rachel Ramirez, founder and director of the Center on Partner Inflicted Brain Injury at the Ohio Domestic Violence Network, has spoken about brain injury and IPV multiple times on podcasts etc.
-
PINK Concussions is the first of its kind to focus on pre-injury education and post-injury care for women and girls with brain injury resulting from intimate partner violence, sports, accidents, or military service.
Some of their efforts in the medical community include organizing international conferences and publicizing current research through the media.
For women and girls, PINK Concussions…
Promotes the use of online communities to reduce the feeling of isolation. There are currently 90+ women enrolled in the international program.
Offers educational resources for schools, sports, and medical clinics
Provides online support groups and weekend retreats for women, girls, parents, caregivers, and medical professionals. There are over 7,500 members across their support groups.
PINK Concussions has developed a YouTube Channel with educational videos on a variety of topics relating to brain injuries in women.
-
SOAR (Supporting survivors through abuse and brain injury through research) is a nonprofit based in Canada working to increase awareness, and improve support and services for survivors through research, education, and advocacy.
They emphasize 3 main goals for their organization:
Explore the intersection of BI and IPV, and its effects through psychosocial and lab assessments
Educate the professionals working with survivors of intimate partner violence by designing training tools that provide the knowledge and skills needed to support those with a TBI.
Empower a community-based support system by providing resources to service providers in health care, brain injury support, and gender-based violence sectors.
-
The Strangulation Training Institute provides a variety of resources and training opportunities for both medical providers and survivors. Their goals include…
Enhancing knowledge and understanding
Improving policies and practices
Maximizing expertise
Increasing accountability of offenders and enhancing the safety of victims
The Strangulation Training Institute provides both in-person and virtual strangulation prevention courses/webinars and ample resources for survivors such as…
Help finding local services
Facts, safety, signs, and symptoms brochures
Imaging recommendations
Danger and strangulation assessment tools
What about COVID-19?
During the pandemic, there were increases in domestic violence cases globally.
IPV severity increased during the pandemic with new cases of IPV that previously had no abuse.
As a result of the pandemic, women experienced:
Economic insecurity and resulting poverty-related stress as a result of the economic crisis, closing of many businesses, and loss of jobs.
Forced-time with partners via quarantine protocols that isolate women with potentially abusive family members.
Disaster-related unrest and instability that can instigate conflicts among partners or families.
Reduced health-service availability and access to first responders due to the preoccupation with COVID-19.
Inability to temporarily escape abusive partners either by economic instability or by the shutdown of many shelters or other resources.
Though the pandemic lockdown has ended, its lingering effects are still being felt, with millions of women coping with brain injuries alongside other pandemic-related impacts. Additionally, understanding how the pandemic has influenced IPV and brain injury is crucial for enhancing future approaches to treatment, resources, support networks, and response strategies for women and IPV survivors in similar situations.
Becoming an Advocate
There are many ways to become an advocate for people experiencing traumatic brain injuries as a result of intimate partner violence. You can advocate for policies such as mandatory screening for TBI in victims of IPV, donate to organizations that help victims of IPV, such as women's shelters, or volunteer your time at crisis hotlines.
In order to become an advocate for somebody in your life who may be experiencing IPV, it's important to know the common signs, as recognition is an important first step. If somebody you know has frequent cuts or bruises, or marks around their neck, it's important to reach out to see if they're in a safe environment.
Other warning signs include drastic behavior changes, seeming uncomfortable around their partner, their partner using rough language with them, or their partner exhibiting controlling behavior. If you notice any of these warning signs in a friend’s relationship or within your own relationships, it is important to reach out to the resources listed at the top of the page and seek help.