Medication
Medications, supplements, and other treatment options can help manage concussion symptoms, but they do not treat the concussion itself as concussions are trauma to the neurons. Therefore, none of the medications listed here treat the concussion itself but instead help address symptoms that follow the concussion.
Many thanks to Elizabeth Sandel, MD, who outlined the importance of exercising caution when using medications to manage post-concussion symptoms.
Important Notes About Medications Used to Manage Symptoms After A Concussion
Additionally, when searching for doctors to prescribe medications to help manage concussion symptoms, try to seek out neurologists, psychiatrists, or PM&R physicians (physiatrists). These doctors have experience treating brain injuries and can become board-certified in brain injury medicine.
Searching “brain injury rehabilitation clinic” can help you find doctors to advise your concussion treatment. We also have information about finding healthcare providers that treat concussions. Finally, it is essential to be aware of potential adverse reactions you might have after taking any of these medications or supplements.
Managing Concussions and Concussion Symptoms
Currently, there are no medications explicitly designed for concussions. This is because concussions are due to damage to the neurons, or cells in the brain, following a blow to the head. Doctors typically will start talking to patients about medications when their concussion symptoms become persistent. For example, doctors might prescribe medications to treat symptoms such as post-traumatic headaches (including migraines), depression, insomnia, etc.
Some people self-medicate with CBD oil from hemp or high CBD/low THC marijuana. Other patients are using over-the-counter medicine, supplements, or caffeine in small doses for headaches.
See the figure below for a breakdown of the types of medications and treatments used to manage symptoms of concussions.
Pharmaceuticals: Over-the-Counter
The Early Period Following a Concussion
Some over-the-counter medications can be used to treat post-traumatic headaches. If you have a headache and suspect a concussion, the Mayo Clinic recommends acetaminophen (Tylenol and other brands).
However, there is concern about taking over-the-counter medications within a short time frame after a concussion because of the rare chance of bleeding in the brain.
The Mayo Clinic also recommends avoiding pain medications that thin the blood, such as aspirin, ibuprofen (Advil, Motrin), or naproxen (Aleve) as they may increase the risk of bleeding. Other sources say not to take acetaminophen until four hours after the concussion and to avoid medications such as Advil and Aleve, which thin the blood, for the first 12 hours of a concussion. We recommend that if your symptoms are worsening, go to the ER. If the doctors suspect bleeding in the brain, they will do scans to rule out that possibility.
Once You Have Ruled Out Bleeding in the Brain
Once any concern about a brain bleed has passed, over-the-counter medications are okay to use for symptoms of a concussion. However, it is also good to be aware of the problems associated with NSAIDs (non-steroidal anti-inflammatory drugs) such as ibuprofen (Motrin and Advil), naproxen (ALEVE), celecoxib (Celebrex), meloxicam, and aspirin.
The recommended dosing on the labels may not be enough to help, and if you take too much, other problems can arise: "non-steroidal anti-inflammatory drugs and aspirin can cause gastritis, gastrointestinal bleeding, increased bleeding time, and peptic ulcer disease." Even more of a concern, "The evidence has been building for years that NSAIDs are bad for the cardiovascular system. Epidemiological studies have suggested that such drugs increase the risk for heart attacks, strokes, congestive heart failure and death."
Therefore, due to the neuronal damage that is part of concussions, we recommend avoiding using NSAIDs to treat post-traumatic headaches.
Acetaminophen (Tylenol) is not an NSAID, and is thus recommended to help manage post-traumatic headaches.
Overall, some over-the-counter medications can help alleviate post-traumatic headaches following a concussion. However, post-traumatic headaches are one part of persistent post-concussion symptoms Prescription and non-pharmacological treatments better address other aspects of Post-Concussion Syndrome.
Pharmaceuticals: Prescription Medications
Doctors may prescribe medications for symptoms such as pain, anxiety, insomnia, and depression. As previously stated, try to seek out neurologists, psychiatrists, or PM&R physicians (physiatrists) to treat concussions and prescribe medications.
Dr. Chris Giza, Director of the Steve Tisch BrainSPORT Program at UCLA, recommends that concussion patients avoid taking medications that create problematic side effects and that medications only be used in conjunction with professional therapies and lifestyle changes.
Headaches
Some prescription medications that can help manage post-traumatic headaches are the tricyclic antidepressants (Amitriptyline, Desipramine, Nortriptyline), triptans, Propranolol, Topiramate, SSRIs, and SNRIs. To learn more about post-traumatic headache treatments that can be administered by a physician, please refer to our Headaches page.
Migraines
Erenumab is an anti-migraine medication that works by preventing the start of the migraine. A study by Jordan VanderEnde and colleagues presented promising results for Erenumab. The drug reduced the headaches of 5 women who developed them after a concussion by 51.1%. While this result is extremely promising, the small participant size indicates that more research is needed to test the efficacy of this migraine medication in managing post-traumatic headaches.
Insomnia
Prescription medications that can help manage insomnia following a concussion are amitriptyline and trazodone. Both medications are generally considered non-addictive, but as always, check with your physician.
Changes in mood
Other symptoms following a concussion are changes in mood. To address mood changes, such as depression or depression-like symptoms, your doctor might prescribe an SSRI, SNRI, valproic acid, or gabapentin.
Cognitive challenges with focus, concentrating, etc.
If you find yourself losing focus and having difficulty concentrating, your doctor might prescribe methylphenidate, which is also used to treat ADHD. Finally, if you are experiencing dizziness or instability, your doctor might prescribe meclizine.
Below is a list of prescription medications that doctors might prescribe to help manage persisting post-concussion symptoms. If your doctor prescribes any of these medications, it is vital to make sure that you’re not taking any supplements or over-the-counter medications that might negatively interact with the prescription medication(s).
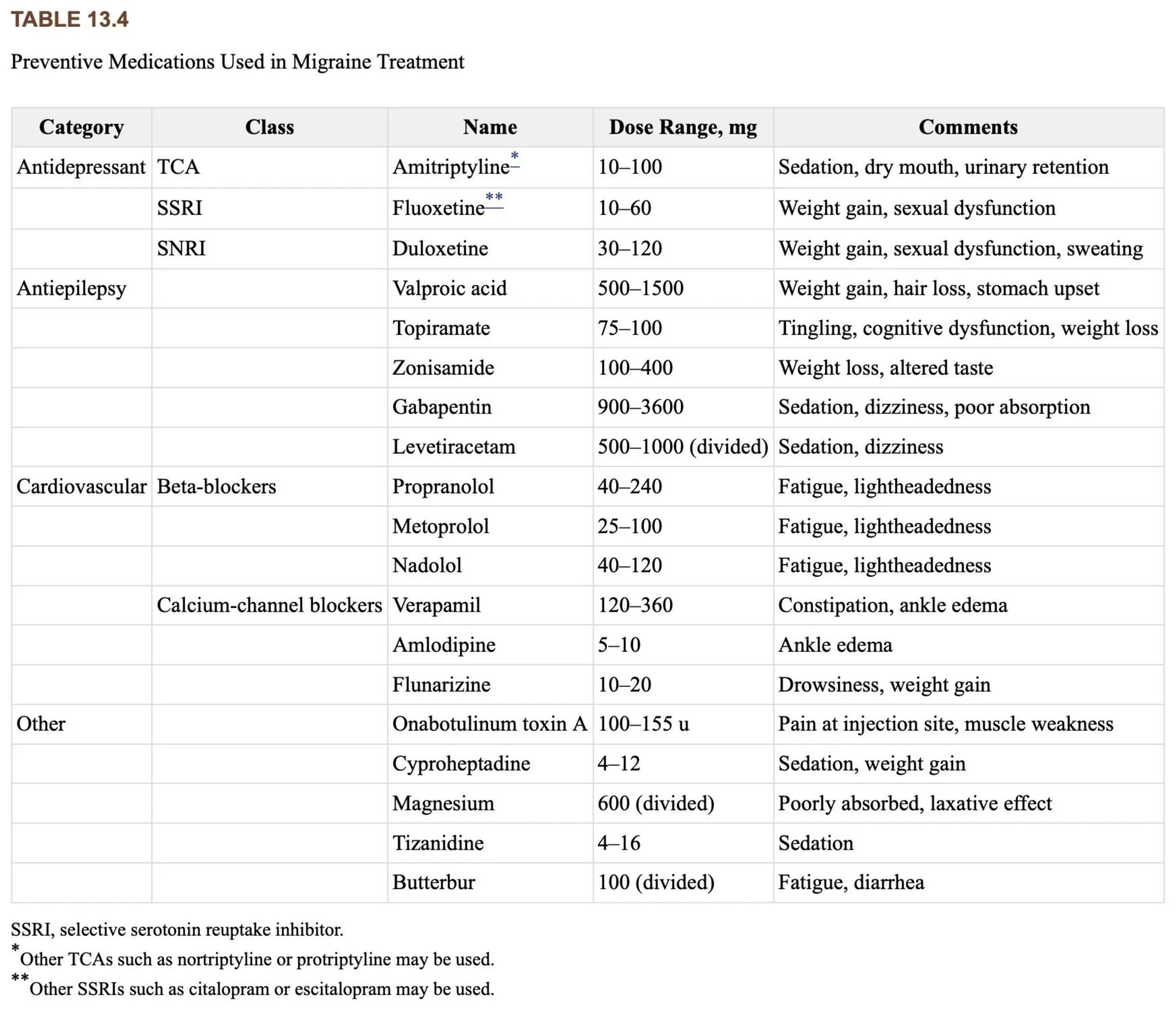
The table is from Brain Neurotrauma: Molecular, Neuropsychological and Rehabilitation Aspects by Sylvia Lucas.
Supplements
In the absence of prescription medications, you might want to try supplements to help manage symptoms of concussion. However, it is important to note that supplements can interact with medications you might already be taking. It is essential to ask your doctor about potential interactions between these supplements and other medications. Additionally, the research surrounding supplements is inconclusive.
The Department of Veterans Affairs lists magnesium oxide as a supplement for managing migraines. Louis Standiford and colleagues completed a randomized cohort study examining the efficacy of PO (oral) magnesium oxide in treating acute concussions in adolescents. They found that oral magnesium significantly decreased concussion symptoms when compared to the placebo group. The main drawback of this study was that they only examined the effects in adolescents.
The Department of Veterans Affairs also lists riboflavin (Vitamin B2) as a supplement that can be taken consistently to help manage migraines. Additionally, some studies suggest riboflavin to be a promising supplement for improving sensorimotor function and spatial memory through reducing neuroinflammation from a traumatic brain injury. One study showed promising results that a high-dose of riboflavin can help treat migraine-type headaches. However, a study by Morris Maizels and colleagues suggests that further research be done to test the efficacy of riboflavin in managing migraines.
Melatonin is produced in the body, but over-the-counter liquid or tablet melatonin can supplement existing melatonin levels. Melatonin may act in the body to support recovery from a traumatic brain injury (TBI), including decreasing neuroinflammation, reducing oxidative stress, improving mitochondrial function, and decreasing glutamate toxicity. It also may have specific therapeutic properties; research has shown it to reduce chronic pain, migraines, headaches, and anxiety. Canadian researchers have found that "children with prolonged PCS,” especially for post-traumatic headaches. A review of multiple studies found similar findings that “there is evidence that melatonin treatment after TBI significantly improves both behavioral outcomes and pathological outcomes.”
The Mayo Clinic notes that melatonin does not cause dependency but is for short-term use only and may have some side effects.
"Melatonin levels rise about two hours before bedtime," according to an article in John Hopkins Medicine. Create optimal conditions for melatonin to do its job by keeping the lights low before bed. Stop using your computer, smartphone, or tablet—these devices' blue and green light can neutralize melatonin's effects. If you watch television, be sure you're at least six feet away from the screen. Turn off bright overhead lights too. Meanwhile, you can help program your body to produce melatonin for sleep at the right time of day by getting exposure to daylight during the morning and afternoon. Take a walk outside or sit beside a sunny window.
Other Treatment Options
Physical therapy is another treatment option that helps manage post-traumatic headaches. The Department of Veterans Affairs lists joint/soft tissue mobilization, cervical joint proprioception training, cervical strengthening, ergonomic/postural assessments, and functional dry needling as effective physical therapies for treating post-traumatic headaches. The VA recommends that beginning these therapies soon after the onset of the concussion increases the chance that the intervention will be successful. For more information about physical therapy, and other non-pharmacological treatments for symptoms of concussions, see our “Treatment and Self-Care” page, which includes cognitive behavioral therapy, vestibular therapy, and graduated exercise therapy among many others.
In the future, there will be more research to determine the best medications for concussions.
We know of two different concussion medications which are in clinical trials. Researchers at the University of Miami, funded by a Canadian R&D firm, are conducting pre-clinical studies of a medication that combines CBD (cannabidiol) and another chemical for use both right after a concussion and for long-term symptoms. See our section on CBD from Marijuana or Hemp for more information about CBD’s role in managing Post-Concussion Syndrome.
Oxeia Biopharmaceuticals Inc is developing a medication based on synthetic human ghrelin (OXE-103) and has just begun clinical trials. The medication is intended to address the brain's metabolic "energy crisis" as it responds to the concussion, with the aim of lessening metabolic dysfunction and therefore preventing the longer-term consequences of concussions. Recently, we interviewed Oxeia’s CEO Michael Wyand and Co-found Dr. Vishal Bansal, where they outlined how OXE-103 works, why it might be effective, and how the clinical trials work.