Resources for School Nurses
Concussions can have physiological effects on brain function, leading to mood changes and cognitive difficulties in addition to the physical symptoms commonly associated with concussion. Concussion, recovery, and persisting symptoms can all affect a student as they begin their return to a classroom and physical activity. In this resource, we'll highlight suggestions for interacting with parents and students, as well as provide resources to help support the student in their return to school and sport.
Concussion definition and implications
Concussions are mild traumatic brain injuries that can occur when the head, neck, or body experiences a blow, resulting in an impulsive force being transmitted to the brain, causing the brain tissue to stretch, compress, and twist inside the skull. Although concussions are an invisible injury, they can significantly impact your overall well-being and mental health. It is essential to recognize that concussions are not just physical injuries; they can also affect your emotions, thoughts, and behaviors.
School nurses can help dispel concussion myths:
Myth: Rest completely in a dark room
Doing this can actually delay recovery! It is better to engage in relative rest, which means engaging in regular, non-strenuous daily activities, including light walking, social interactions, or easy household chores. Mild and brief symptom worsening is okay, but be mindful of current guidelines.
Myth: Stay off of screens until recovered
Screen use (phones, TVs, computers, etc.) should be minimized for the first 48 hours (130 minutes total over two days) but can be increased as tolerated afterward. Maintaining social connections, even over the phone, is an important part of the recovery process!
Myth: Wait for symptoms to resolve completely before returning to school
Students do NOT need to be asymptomatic or medically cleared to return to school! Students should return to school within a week, with the help of adjustments or accommodations such as modified schedule, workload, and classroom environment.
What to do when a student comes into your office with a concussion
Identifying Concussion
See CDC Factsheet for full list of signs and symptoms
Commons signs include:
Confusion, memory and concentration issues, feeling foggy
Poor balance, dizziness, nausea
Inability to remember events before or after incident
More irritable, nervous, anxious
More emotional
Common symptoms include:
Headache
Fatigue
Blurred vision
Light and sound sensitivity
CALL 911 IN CASE OF…
loss of consciousness, or deteriorating consciousness
increased confusion or agitation, combativeness
drowsiness or inability to wake up
significant nausea or repeated vomiting
convulsions or seizures
slurred speech or limb numbness
headache that worsens and does not go away
loss of vision or double vision
Note: Not every concussion leads to immediate symptoms - symptoms may appear hours or even days after the injury.
Immediate care
Allow child to rest
Even if they say they feel fine, a student displaying signs of concussion should NOT return to class or sport. Do not provide painkillers within 12 hours of concussion, as they may mask worsening symptoms and medications like ibuprofen and aspirin may increase risk of bleeding.
Don’t allow the student to leave school by themselves, drive, or ride a bike.
Inform family as soon as possible
Advise families to allow their child 1-2 days of relative rest, meaning engagement in non-demanding tasks such as easy daily chores and light walking, with extremely limited screentime in the first 2 days.
Advise family to see healthcare professional as soon as possible
Family should seek out a complete evaluation and diagnosis within 2 days so they can determine next steps for recovery (which healthcare professionals are allowed to diagnose concussion varies by state).
Helping in return to class
Students may need help securing accommodations or adjustments (postponing tests, extra time on assignments, partial school days) in order to participate in class.
Students may also need to use the resources provided by the nurse’s office to rest from class.
If symptoms last 10 days or longer
If you notice symptoms persist further than 2-4 weeks, recommend seeking additional care. Guidelines recommend seeking treatment if headaches, dizziness, and neck pain last longer than 10 days.
What to tell parents
Remain calm - while concussions are serious, it is important that parents remain calm, as higher parental stress has been linked to prolonged recovery.
Recommend they visit a healthcare provider within two days. Types of professionals that can give official diagnoses vary by state.
There are many myths about what constitutes adequate concussion care.
See this CATT pdf, Concussion Resources for Parents and Caregivers, for a more comprehensive review.
-
Suspected concussion? Next steps
Be sure to visit a healthcare professional within the first 2 days.
1) Relative (not strict) rest begins immediately and for up to 2 days
2) Engage in light physical/cognitive exercise as tolerated
3) Gradually increase intensity of activities
4)Full return to learn
5)Full return to sport with medical clearance
Common Myths:
Myth: Rest in a dark room.
Doing this can actually delay recovery! It is better to engage in relative rest.
Myth: Don’t use screens.
Screen use should be minimized for the first 48 hours, but is okay afterwards.
Myth: Wait for symptoms to resolve before returning to school
Return to school within a week with the help of adjustments or accommodations.
Red Flag Symptoms: SEEK CARE IMMEDIATELY
- Neck pain or tenderness
- Seizure, ‘fits’, or convulsion
- Loss of vision or double vision
- Loss of consciousness
- Increased confusion or deteriorating conscious state (becoming less responsive, drowsy)
- Weakness or numbness/tingling - in more than one arm or leg
- Repeated vomiting
- Severe or increasing headache
- Increasingly restless, agitated, or combative
- Visible deformity of the skull
Advice for persisting symptoms
If symptoms persist, tell parents it is important to seek targeted care:
In the first 10 days after concussion, sleep disturbance is associated with increased risk of persisting symptoms and may warrant further evaluation and treatment.
If headaches, dizziness, and/or neck pain last longer than 10 days, advise parents to seek rehabilitative care.
If symptoms last longer than 4 weeks, further treatment including collaborative care is recommended.
Protocol for return to school/sport
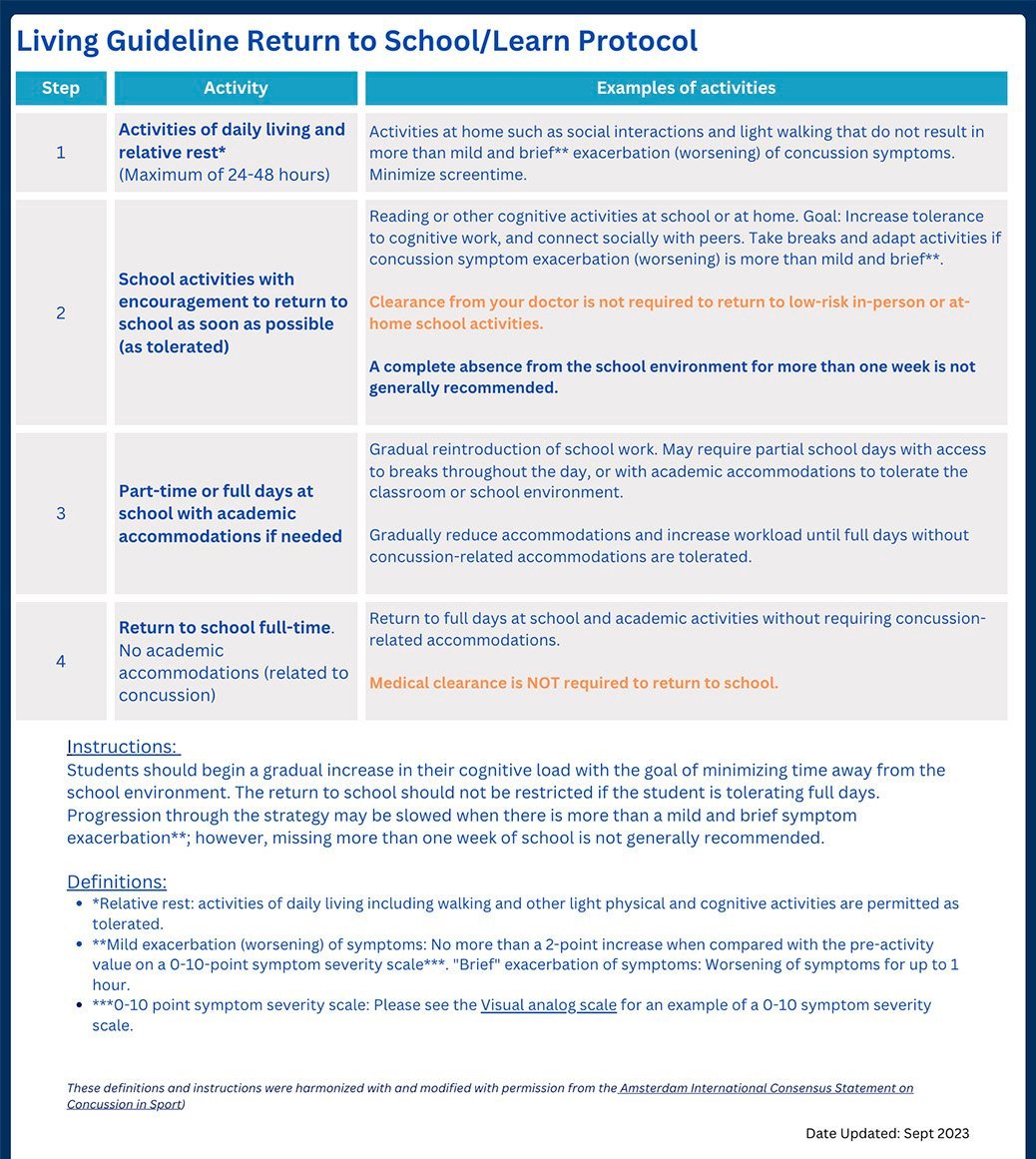
These guidelines are adapted from the Amsterdam International Consensus Statement on Concussion in Sport and pedsconcussion.com.Return to School
Concussion incident: day 0
Days 1-2
Engage in relative rest at home: activities of daily living like easy walking and other light social and cognitive activities. Minimize screen time.
As soon as tolerated (at home)
Reading or other cognitive activities at home. Any activity where symptom exacerbation is mild and brief is “tolerated”. Engaging in as much cognitive activity as is tolerated will help ensure a faster return to school and normal cognitive functioning. Absence from school for more than a week is not recommended.
Within one week
Return to school part-time and/or with academic accommodations or adjustments. No doctor’s note is required for return to school.
As soon as tolerated (at school)
Full return to school. If the student is experiencing persisting concussion symptoms, some academic accommodations may remain in place to support them.
For more details, check out the PedsConcussion guidelines by clicking on the image above.
Return to Sport
Concussion incident: day 0
Days 1-2:
Engage in relative rest: activities of daily living like easy walking and other light social and cognitive activities. Minimize screen time.
Day 3:
Begin aerobic exercise: beginning with walking at a slow to medium pace, stationary cycling, or other low-intensity age-appropriate activities; aim to exert light effort (up to 55% of maximum heart rate). Take breaks and modify activities as needed to increase/decrease intensity of aerobic exercise. Refrain from participating in sport-specific activities. Avoid activities with risk of inadvertent head impact.
As tolerated: increase effort of aerobic exercise
Continue aerobic exercise, working up to moderate effort (up to 70% of maximum heart rate).
As tolerated: low-risk sport-specific activity
Increase intensity of activity while introducing low-risk sport-specific actions and change of directions. Avoid activities with risk of inadvertent head impact.
Before further increasing training intensity, medical clearance and full return to school are required.
Then, gradually:
Begin non-contact training drills and activities, resuming usual intensity of exercise, coordination, and activity-related cognitive skills.
Return to all non-competitive activities, all gym class activities, and full-contact practices. While avoiding competitive gameplay, “restore game-play confidence and have coaches assess functional skills.”
Finally, return to sport with normal, unrestricted competitive gameplay, school gym class, and physical activities. Medical clearance is required before student can return to sport - the specific medical providers that can provide clearance vary by state.
For more details, check out the PedsConcussion guidelines by clicking on the image above.
How to determine an effective level of activity effort – what is mild symptom exacerbation?
The mild exacerbation (worsening) of symptoms due to physical activity is defined as follows:
Prior to beginning an activity, rate symptom severity on a 10-point scale. While doing the activity, symptom severity should not increase by more than two points, and symptom level should return to pre-activity baseline within one hour.
A mild exacerbation (worsening) of symptoms due to physical activity, as described above, does not delay recovery. Do not engage in activities that result in more than a mild worsening of symptoms. If any activity results in more than a mild worsening of symptoms, cease to perform that activity and attempt the next day.
Concussions are serious issues, and parents and students alike may depend on support from a school nurse. It is important that the latest guidelines are followed to help get the student on track for a return to school.
Recommended resources
CDC Heads Up offers a fact sheet for nurses that outlines this information.
Pedsconcussion.com offers many fact sheets outlining this information.
CATT online offers a guide for families and school professionals.
References used to make this resource
“Concussion Awareness Training Tool.” https://cattonline.com/
Lumba-Brown, A., Yeates, K. O., Sarmiento, K., et al. “Centers for Disease Control and Prevention Guideline on the Diagnosis and Management of Mild Traumatic Brain Injury Among Children.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7006878/
Mayo Clinic “Concussion.” https://www.mayoclinic.org/diseases-conditions/concussion/diagnosis-treatment/drc-20355600
Patricios, Jon S. et al. “Consensus statement on concussion in sport: the 6th International Conference on Concussion in Sport–Amsterdam, October 2022.” https://bjsm.bmj.com/content/57/11/695
Teel, E. F., Caron, J. G., & Gagnon, I. J. “Higher parental stress is significantly related to longer clinical recovery times in concussed children: A mixed-methods study.” https://pubmed.ncbi.nlm.nih.gov/34518082/
Zemek, R., Reed, N., Dawson, J., et al . “Living Guideline for Pediatric Concussion Care.” www.pedsconcussion.com