Light Therapy Promotes Neurological Resilience in College Football Players
Image credit: Lindsey HM, Esopenko C, Jain D, et al. Transcranial Photobiomodulation Promotes Neurological Resilience in Current Collegiate American Football Players Exposed to Repetitive Head Acceleration Events. Journal of Neurotrauma. 2026;0(0). doi:10.1177/08977151251403554.
By Malayka Gormally. This article was initially published in the 2/5/26 Edition of our Concussion Update newsletter; please consider subscribing.
Contact sport athletes risk not just concussions, but the cumulative effects of repetitive head acceleration events (RHAE), which include direct hits to the head and blows to the body that transmit forces to the brain. RHAE exposure contributes to neuroinflammation and decreased white matter integrity in even one season of participation in contact sports, and cumulative RHAE over years appears to increase the risk of neurodegenerative disease, including chronic traumatic encephalopathy (CTE). What can be done to reduce the neurodegenerative risks from contact sports?
In a first-of-its-kind study with active college football players, researchers investigated the potential impact of a transcranial photobiomodulation (PBM) intervention, using a commercially available headset to deliver near-infrared light to the brain through the skull. The PBM intervention resulted in sustained microstructural stability in athletes' brains throughout a 16-week college football season, including preseason training. In contrast, the brains of athletes who received a sham PBM treatment showed marked increases in neuroinflammation and axonal damage, and a reduction in white matter integrity, by the end of the football season.
Published in the Journal of Neurotrauma, the double-blinded study compared pre- and post-season diffusion MRI scans of 26 NCAA Division 1 football players. Their findings suggest that “By mitigating the microstructural changes associated with RHAE, PBM may reduce the risk of long-term neurological impairment and enhance the safety of sport participation.” In a University of Utah press release, lead author Dr. Hannah M. Lindsey remarked, “My first reaction was, ‘There’s no way this can be real. That’s how striking it was.’” Concussion Alliance recommends this 2-minute news report from KSL News Utah.
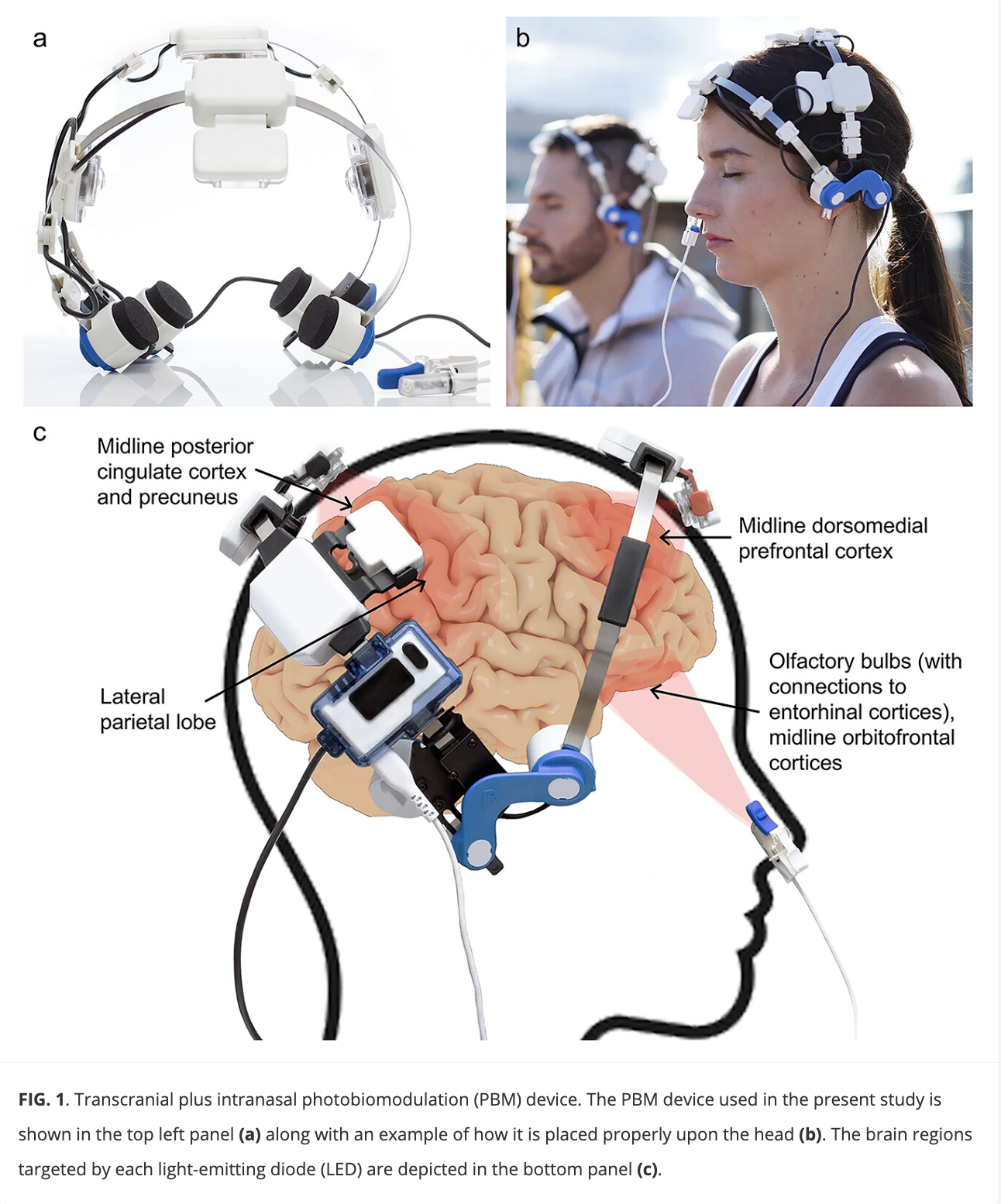
How does PBM positively affect the brain? The authors cite prior research findings that PBM interventions “reduce neuroinflammatory signaling, enhance mitochondrial function, increase cerebral blood flow, and facilitate neuroplasticity.” For the intervention, the researchers used the Vielight Neuro Gamma, a commercially-available headset with four specialized LEDs that deliver 810 nm near-infrared light, pulsed at 40 Hz, through the skull to the brain. Attached to the headset is a nasal clip with an LED that delivers near-infrared light through one nostril into the frontal lobes of the brain. The sham version of the device did not deliver near-infrared light (which is invisible to the eye). The athletes self-administered the treatment (either PBM or sham) for 20-minute treatments three times a week, overseen by the research staff. They used the 2020 Neuro Gamma version 3, following the Vielight-recommended protocol at the time, which was 3 times per week.
The study authors refer to Vielight’s new suggested protocol of 5-6 times per week, recommending that “Future studies should incorporate these updated protocols and explore newer PBM devices with additional targeting capabilities, such as direct cerebellar illumination.” Concussion Alliance notes that the currently available version, the Vielight Neuro Gamma version 4, adds an LED light at the back of the head that targets the cerebellum, and so is likely the device the authors are referring to. (Concussion Alliance has no affiliation with Vielight.)
While this study did not address functional outcomes, such as pre- and post-season cognitive function, the authors note that chronic neuroinflammation has been implicated in cognitive dysfunction, disrupted sleep, and mood disturbances. The authors note that “By mitigating inflammatory responses, PBM may help preserve the neural circuitry critical for cognitive function, emotional regulation, and restorative sleep.” On this topic, some of these same researchers recently published a study on PBM and cognition. In our synopsis of this study, we wrote that 8-10 weeks of at-home treatment with a transcranial photobiomodulation (tPBM) device resulted in statistically significant improvements in cognitive function in adults exposed to repetitive head acceleration events (RHAE).
For this current study, Lindsey et al. note that “longitudinal studies that follow athletes over multiple seasons” are needed to determine if PBM “could potentially reduce the cumulative burden of neuroinflammation that contributes to long-term neurodegenerative risk.” Limitations of this study include the small sample size and the lack of a control group of athletes in limited-contact or non-contact sports.