
Persisting Symptoms
After Concussion
Previously called “Post-Concussion Syndrome” or PCS
Symptoms that persist for more than 4 weeks after a concussion are considered persisting symptoms; it is important to seek rehabilitative treatment for these symptoms. (For some symptoms, patients should seek care during the first four weeks.) Approximately one-third (10% and 30%) of concussion patients experience persisting symptoms after a concussion.
Concussion Alliance Advisory Board Member Sara Etheredge, PT, DPT, CKTP, CCI, CMTPT, AIB-VRC, from the Concussion Care Centre of Virginia, has reviewed this page for content accuracy.
Contents
Overview
Why not use the term “post-concussion syndrome”?
While post-concussion syndrome (PCS) is the term many people still use, the new term used by researchers and clinicians is persisting symptoms after concussion (PSaC).
The reason for the change is that each person who sustains a concussion will have a different combination of symptoms. In contrast, “syndrome” means a group of symptoms that always occur together.
Timeframe for persisting symptoms
According to the most recent international consensus, symptoms persisting after 4 weeks are considered persisting symptoms.
How common is it to develop persisting symptoms?
The most commonly accepted statistic is that 10-30% of concussion patients develop persisting symptoms. For example, a 2016 study found that approximately one-third of pediatric concussion patients experience persisting symptoms. A 2018 study estimated that between 11.4% and 38.7% of people with concussions will develop persisting symptoms.
However, a few studies have found even high rates, such as a 2022 study found that “50% reported three or more symptoms at a year after their injury, and >70% reported at least one problematic symptom.”
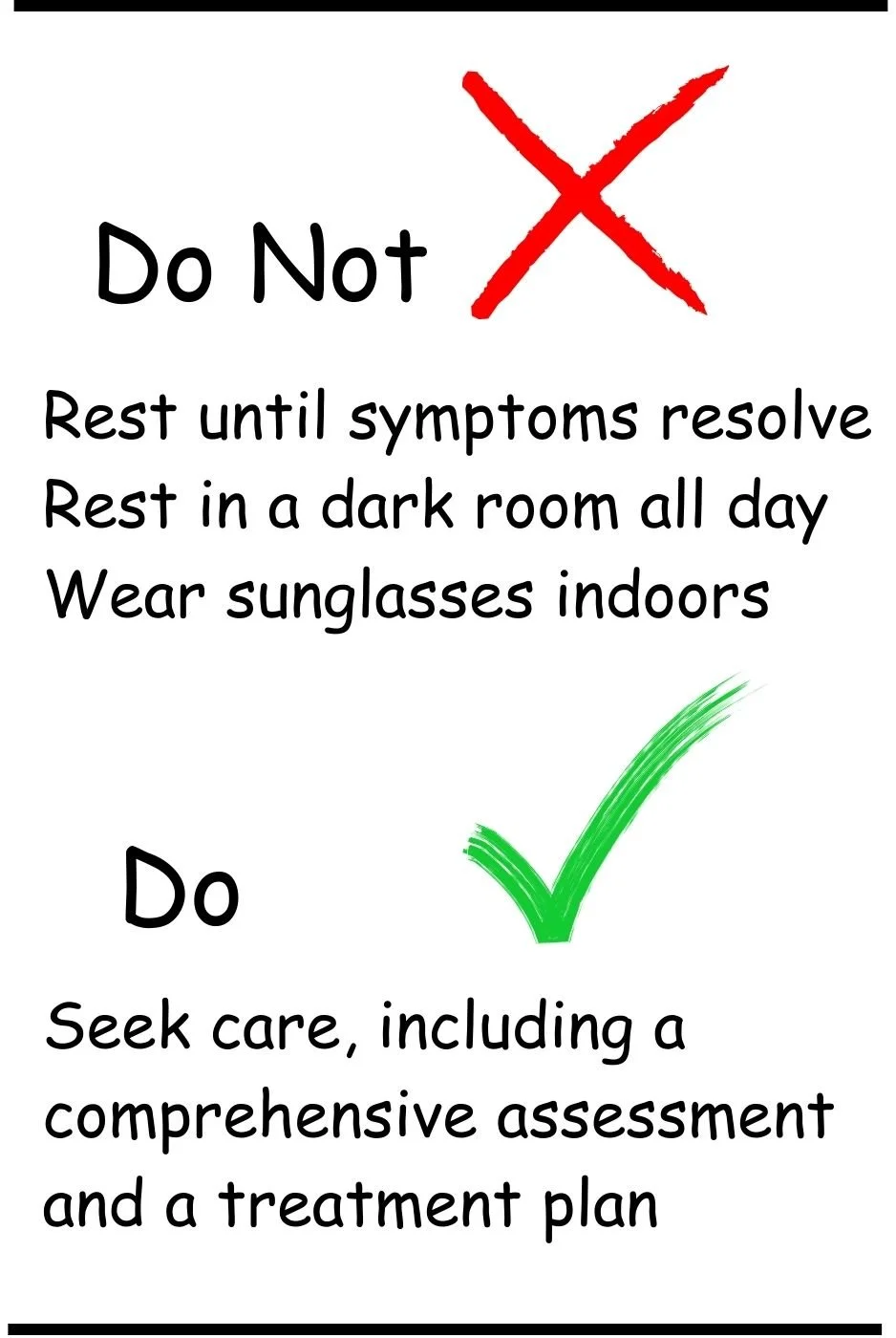
Avoid outdated advice
Do Not:
Rest until symptoms resolve
Rest in a dark room all day (called “cocooning”)
Wear sunglasses indoors
All these tactics have been found to SLOW recovery.
Do:
Seek care for persisting symptoms, including a comprehensive assessment and a treatment plan. See our next sections for more information.
Quick Guide
Our double-sided “quick guide” covers central concepts about persisting symptoms after concussion. Click here or on the quick guide images to download a PDF.
Persisting symptoms and how they can affect your life
Please read more about how persisting symptoms after a concussion can affect your life in our resources The Invisible Injury, Mental Health, and Mental Health Among High Schoolers.
Four categories of persisting symptoms
Physical (including vision)
Headache
Sensitivity to light
Sensitivity to sound
Fuzzy, double, or blurry vision
Trouble with reading or looking at screens
Trouble with scrolling on devices
Dizziness
Balance problems
Trouble tolerating riding in a car
Overwhelm or fatigue in busy, crowded, noisy, or visually complex environments
Ringing in the ears
If you have neck pain, dizziness, or headaches that persist beyond the first week:
Seek cervicovestibular therapy with a physical therapist. Patients with dizziness or balance problems may benefit from vestibular therapy in addition to cervicovestibular therapy. See our resources on Physical Therapy and Vestibular Therapy. Our Occupational Therapy resources may also be useful.
Medication to help with headaches, sleep issues, or challenges with mood is sometimes appropriate. Learn more about medications in our Medications and Neurologist resources.
If you have vision problems that persist for more than 4 weeks, including trouble reading and looking at screens:
Seek vision therapy; see our Vision Therapy resource.
Cognitive
Difficulty with memory
Difficulty recalling events & information
Difficulty with attention
Getting distracted easily
Difficulty with focus and concentrating
Difficulty with thinking clearly
Simple tasks now feel difficult
Confusion
Feeling slowed down
Feeling mentally “foggy”
If you have difficulty with memory, concentrating, or thinking clearly that persists for more than 4 weeks:
Seek assessment and cognitive rehabilitation from a neuropsychologist or speech-language pathologist. Often these specialists work at outpatient rehabilitation clinics–learn more.
To learn more about cognitive dysfunction after a concussion, assessment, rehabilitation, and the types of healthcare providers who can help:
Sleep
Sleeping less
Trouble falling asleep or staying asleep
Irregular sleep patterns
Waking up feeling unrested
Fatigue or drowsiness during the day
Sleeping more than usual (common with a recent concussion)
If you have problems with sleep that persist for the first 10 days after a concussion or longer, it’s important to see a sleep specialist. See our resource on Sleep and Sleep Problems.
Mood/Behavioral
A concussion patient can develop new mood and behavioral challenges after a concussion, or their pre-existing mental health issues may increase or change.
Increased Irritability
Becoming frustrated or upset more easily
Increased depression
Feeling worried, sad, or hopeless
Increased anxiety
More emotional
Crying more easily or feeling overwhelmed
Increased apathy or lack of motivation
Reduced tolerance to stress, emotional excitement, or alcohol
Reduced tolerance in these areas could be due to cognitive or emotional stressors
Seek care as soon as possible for issues related to mental health. Learn more about mental health challenges after a concussion, how to find help, and types of treatments, such as cognitive behavioral therapy. We have several resources with information.
Persisting emotional symptoms are caused by multiple factors
A person who sustains a concussion is at increased risk for emotional (mood) symptoms after a concussion. This risk for emotional symptoms increases if you develop persisting symptoms after a concussion. There are primary and secondary factors for emotional symptoms after a concussion.
Primary factors for emotional symptoms after a concussion
Emotional symptoms are due to the concussion itself, such as irritability, mood instability (mood lability)
Secondary factors for emotional symptoms after a concussion
All the difficulties around concussion being an invisible injury: see our Invisible Injury resource.
Uncertain timelines for when you will be fully recovered, when you can return to sport
Social impacts, for example, social isolation, missing out on sports or activities
Academic impacts on grades, SAT testing, and scholarship opportunities
Work impacts such as missing work, potential job loss, reduction or loss of income, loss of social connections at work
The resource for this section is from a 2025 clinical webinar presented by Christina L. Master, MD, FAAP, CAQSM, FACSM, and the Minds Matter Concussion Program at the Children’s Hospital of Philadelphia.
Aerobic exercise therapy reduces persisting symptoms
An aerobic exercise therapy program can reduce persisting symptoms after concussion. A 2024 study found that “A 12-week aerobic exercise intervention improves overall symptom burden, quality of life and specific symptom domains in adults with PPCS [persistent post-concussion symptoms]”
Guidelines recommend combining aerobic exercise therapy with other types of treatments for persisting symptoms, which you can find below. Always consult a physical therapist to determine what is appropriate for you. For more information on how to try aerobic exercise therapy safely, click the button below.
Where to get care for persisting symptoms
Ask for a referral to a clinic that will do a comprehensive assessment to identify issues within the different symptom domains: physical, cognitive, sleep, and mood. In other words, what type of symptoms do you have, and what might be contributing to these symptoms? Learn more about this in our section Assessment for persisting symptoms (below). After the assessment, an individualized treatment plan may include physical therapy, cognitive rehabilitation, referrals to mental health specialists, and other types of treatments..
Some concussion clinics have these resources. However, sometimes the best option is to get a referral to an outpatient rehabilitation clinic affiliated with a hospital. These clinics typically have many of the specialists necessary for concussion treatments, such as physical therapists, occupational therapists, speech language pathologists (SLP), etc. Learn more about choosing a clinic here: Concussion and Rehabilitation Clinics.
Assessment for persisting symptoms
Various systems in the body can be affected by persistent symptoms, so an assessment for persisting symptoms needs to be broad and comprehensive. Additionally, a collaborative approach between different specialists is often needed in these cases.
This section draws in part from a 2025 virtual presentation by Sara Etheredge, PT, DPT, CKTP, CCI, CMTPT, AIB-VRC
History
Your doctor will ask questions about:
The specific incident that caused the concussion
Symptoms felt at the time of the injury and how they have changed over time
Previous history of migraines/headache, neck pain, sleep problems, anxiety, medications, etc.
Questionnaire and screening tools
Your doctor may have you take a symptom questionnaire, such as the Concussion Clinical Profiles Screening Tool. This questionnaire will help your physician understand your symptom profile. Symptom profiles include cognitive-fatigue, ocular (eye), vestibular (balance or dizziness), mood (such as anxiety or depression), cervical (neck), and migraine.
Your doctor may have you take one or more psychosocial screenings (questionnaires) to assess for emotional and mood disturbances, such as anxiety or depression.
Examination
Your doctor, physical therapist, or other concussion specialist may check your:
Neck function, such as movement, tenderness, strength, etc. See our resource on Physical Therapy for more information about the neck.
Balance and vestibular function. See our resource on Vestibular Therapy.
How your eyes are functioning, called oculomotor function: this includes how well your eyes track an object side to side, how well they focus on an object as it gets close to your eyes, etc. See our resource on Vision Therapy.
Autonomic nervous system (ANS): check for problems with the ANS, including tests of orthostatic vitals, heart rate variability testing, 10-minute stand test, and marching test. See our resource Autonomic Nervous System Dysfunction.
Assessment of the autonomic nervous system may include testing for exercise intolerance, as measured in a graded aerobic exercise test, such as the Buffalo Concussion Treadmill, Bicycle, or Marching Tests for assessment of exercise tolerance. Read more on our Aerobic Exercise Therapy page.
Brain function (memory, ability to process information, reaction times, etc.)
Special tests may sometimes be required
Formal neuropsychological testing to further assess brain function. Read more about neuropsychological testing here.
Neuroendocrine screening for hormone imbalances, see our resource on Hormone Therapy.
Test for benign paroxysmal positional vertigo (BPPV)
Conventional Imaging
CT and MRI scans are usually normal for concussions. Since CTs expose the patient to radiation and MRIs are expensive, doctors use these imaging methods sparingly.
A CT or MRI may be used to rule out underlying structural brain injury, such as a brain bleed (hematoma).
Ultimately, imaging can be used to help reassure your doctor that they are not missing a structural injury, such as bleeding in the brain.
Advanced Investigation Techniques: only available to researchers
PET scans, functional MRI, Blood biomarkers, etc.
All advanced investigation techniques show “changes” in concussed individuals when compared to non-injured “controls”
**This section on advanced investigation techniques summarizes information from the University of Calgary and Université Laval’s Massive Open Online Course (MOOC) on concussions
What makes a person more vulnerable to persisting symptoms?
Certain acute symptoms
“Acute symptoms” means symptoms that occur in the first 72 hours after a concussion.
Your medical history
Delay in getting appropriate care of the concussion
Pre-existing conditions (before the concussion)
Migraine headaches
Attention deficit hyperactivity disorder ADHD and attention deficit disorder ADD
Learning disabilities
Sleep disorders
How the concussion happened
Who you are
Children 8-12 years old
Teenagers 13-18 years old
Elderly adults










































Results from a recent study published in the Clinical Journal of Sports Medicine indicated that youth with exercise-induced vision dysfunction following sport-related concussion were at “a 3-folder greater risk” of developing persistent post-concussive symptoms (PPCS) compared to those without exercise-induced vision dysfunction.