Common pain relievers show promise in speeding concussion recovery (7/17/25 Newsletter)
In this newsletter: Opportunities, Concussion Alliance Lunch & Learn, Therapies & Diagnostic Tools Under Research, Self-Care, Youth, Reader Feedback: Dual-task and Neuromuscular Training
Writers: John Rosseel, Sofia Lozano, Marina Oljaca, and Heather Campbell
Editors: Conor Gormally & Malayka Gormally
Do you find the Concussion Update helpful? If so, forward this to a friend and suggest they subscribe.
Opportunities
Monday, July 21, 12-2 pm EDT: A webinar, Minds Matter Concussion Model: Acute Clinical Concussion Management, "is open to anyone responsible for implementing a concussion protocol following injury," and all participants will receive an evaluation and treatment toolkit. Presenters include Christina L. Master, MD, who is considered one of the top clinician–researchers in this field. General admission (no continuing education credits) is $30. CEUs are available for ATs, Nurses, PTs, and Physicians; tickets range from $45 to $75.
Wednesday, August 13, 6 pm EDT: A webinar, Getting Things to Stick: Strengthening Memory and Habits after Brain Injury, presented by Stephanie Wagner, Director of Learning & Development at Healthy Minds Innovations, and hosted by the nonprofit LoveYourBrain. Register in advance: there is a sliding scale fee starting at free.
Summer Concussion Alliance Lunch & Learn
July 24: Join Concussion Alliance Co-Founders for an Open Q&A!
On July 24th at 1 PM PST | 3 PM CST | 4 EST, join Concussion Alliance Co-Founders Conor Gormally & Malayka Gormally for our second virtual Lunch & Learn webinar! This Lunch & Learn will be an open Q&A with Conor and Malayka, so bring on your concussion questions! Note: We are unable to answer any personal questions about an individual’s specific medical issues, and these answers do not constitute medical advice.
Therapies & Diagnostics Under Research
Enzyme inhibitor after TBI in mice protects the blood-brain barrier, preserves cognition, and reduces the risk of long-term neurodegeneration
A study by Yeojung Koh et al. found that inhibiting the enzyme 15-PGDH could protect the blood-brain barrier (BBB) and negate neurological impacts from traumatic brain injury (TBI). The BBB filters out bacteria and unwanted proteins from entering the brain, but may become damaged after a TBI (BBB damage is also present in aging, Alzheimer's, and CTE pathology). Using mouse subjects with TBI, the authors found that TBI is associated with an increase in 15-PGDH. (Note: there was no mention of mild TBI, so the TBIs were likely moderate-severe.) The authors also found elevated 15-PGDH in mice models of Alzheimer's and aging (older mice). After inhibiting the 15-PGDH enzyme with injections, the mice with TBI did not show any loss of memory or motor function compared to their healthy counterparts. The study, published in the journal Proceedings of the National Academy of Sciences of the United States of America, asserts that the appropriate level of 15-PGDH in the brain acts as a "guardian for BBB integrity", offering protection from neurodegenerative disease. The authors argue that inhibiting 15-PGDH could be a "therapeutic target" for TBI as it protects the BBB and completely preserves cognitive function in mice.
15-PGDH is an enzyme that is enriched in the BBB and has many functions in the cells within this region. However, the authors found that an overabundance of 15-PGDH is a common factor in aging and neurodegenerative diseases such as Alzheimer's. In the short term, too much 15-PGDH can lead to common TBI symptoms such as loss of memory, and motor function––in addition to affecting BBB structure. This study used a 15-PGDH inhibitor, (+)-SW033291, in the mouse subjects, injected twice daily beginning twenty-four hours after their TBI and continuing for 21 days. Between days 14 and 18, the mice were given the Morris Water Maze test to assess their memory and cognitive functions. After three weeks, researchers studied the mouse brains to find changes in brain chemistry and structure. The authors found that, unlike common TBI outcomes, the inhibitor prevented severe damage to brain cells after three weeks, maintained the integrity of the BBB, mitigated inflammation, and fully preserved cognitive function (as demonstrated in a water maze test) to the point that the mouse subjects were indistinguishable from healthy controls. Koh et al. suggest that this may result in a lesser chance for age-related diseases like Alzheimer's to appear later in life following a TBI. They argue that further research is needed to understand the role of 15-PGDH, especially in the BBB, to determine the safety of human trials in the future.
Self-Care
Common pain relievers show promise in speeding concussion recovery
People who take over-the-counter pain relievers after a concussion may recover faster than those who do not take pain relievers. Over-the-counter pain relievers such as acetaminophen or ibuprofen are non-steroidal anti-inflammatory drugs commonly used to reduce pain, inflammation, and fever. An article in Lab+Life Scientist discusses a preliminary study presented at the American Academy of Neurology’s 77th Annual Meeting in April, 2025 that explored OTC pain relievers in concussion recovery. The research, conducted by Dr Kyle Arnold et al. with the NCAA and the U.S. Department of Defense CARE Consortium, involved over 1,600 NCAA athlete and military cadet concussion patients. It compared recovery outcomes between those who took OTC pain relievers shortly after injury and those who did not. The study authors identified improvements due to OTC pain relievers after concussion in three areas: faster time to return to activities with no restrictions, faster time to being symptoms free [or faster time to full resolution of symptoms], and reduced severity of symptoms. An ANN press release on this study emphasized that OTC pain relievers are accessible and cost effective options that may benefit concussion recovery. However, Dr Kyle Arnold et al. cautions that these findings are preliminary and call for further validations through controlled trials to confirm the safety and effectiveness of pain relievers during concussion treatment. This study opens the door for reconsidering pain management strategies in concussion care to potentially improve patient outcomes.
Time to clearance to return to activities with no restrictions
Results of the study showed that people who took the pain relievers were 20% more likely to be cleared to return to activities with no restrictions earlier than those who did not take pain relievers. The study also concluded that individuals using OTC pain medications returned to unrestricted activities about two days earlier by the time 50% of the study participants were fully recovered and seven days earlier by the time 90% were recovered.
Time to resolution of symptoms
People who took pain relievers were about 15% more likely to have their symptoms more quickly than those who did not take pain relievers. Symptoms resolved one day sooner in the pain reliever group by the time 50% of all participants had recovered and three days sooner by the time 90% had recovered.
Severity of symptoms
Those who took pain relievers also scored lower on tests of how severe their symptoms were overall and how severe their headaches were.
Timing of when to take OTC pain relievers
The authors concluded that the earlier people took the pain relievers after the injury, the faster they recovered. Starting pain relievers early (on the first day after concussion) was associated with an average of eight days faster recovery than those who began taking pain relievers five or more days post-injury. The difference in the type of pain reliever, whether acetaminophen or ibuprofen, did not significantly impact recovery speed.
Youth
One childhood concussion lowers the chances of higher education by 15%
A retrospective cohort study by Möttönen et. al at Tampere University in Finland, published in the European Journal of Epidemiology, found that all-severity pediatric traumatic brain injury, including concussion (pTBI), is associated with lower educational attainment. Using data collected in the Finnish Care Registry for Health Care between 1998 and 2018, the researchers compiled information on all individuals aged 0-17 years in Finland who were at least 26 years old at the end of follow-up. This formed a pTBI group of 8487 patients that included all severities of TBI, the vast majority (89.5%) of which were concussions. Patients with pTBIs had considerably lower educational attainment at all levels of higher education than the reference group. Additionally, those with specific intracranial injuries (moderate to severe TBIs) were less likely to have attained any tertiary education (undergraduate or graduate) compared to those with concussions. These findings could indicate a dose-response relationship between TBI and later educational outcomes, with more severe injuries associated with lower educational attainment. However, even one mild TBI (concussion) lowered the chances of higher education by 15%, and reduced these individuals' rate of attaining the highest levels of education (graduate education) by 19%. In a New Atlas article, lead author Dr. Möttönen emphasizes that while a single concussion is often considered a relatively harmless event, their "research suggests that it can have long-term effects on learning and cognitive abilities", indicating the need to focus on TBI adjustments and accommodations in school and healthcare settings.
The pTBI group consisted of 7594 patients with concussion and 892 patients with moderate to severe TBI, while the reference group included those with ankle and wrist fractures. The authors divided L=levels of education into: upper secondary (12 years), lower tertiary (15 years), and higher tertiary (17 years or more). The pTBI group did not move from upper secondary education to tertiary education as often as the reference group. Similarly, the pTBI group did not move from lower tertiary education to higher tertiary education as often as the reference group. In contrast to the reference group, the pTBI group was more likely to pursue vocational training rather than upper secondary education.
The study was limited by the lack of information on pTBI severity and people who missed upper secondary education. Additionally, confounders such as parental education, living in a neighborhood or urban area, or other prior mental or physical morbidity were not considered in the analyses.
Reader Feedback: Dual-task and Neuromuscular Training
A physical therapist and educator wrote to comment on topics in our previous newsletter (7/10/25), adding information about blending scientific info and narrative in concussion education, neuromotor retraining via multi-task challenges, and neuromuscular training
Dear Conor,
I always enjoy reading through the highlights you send. I was particularly pleased with the education article touting a mix of scientific info and narrative when teaching about concussion. I lead a concussion sub-module in the Regis University advanced practice Orthopaedic Physical Therapy Residency program, and I used to teach a module under Differential Diagnosis in the doctoral PT program, as well. A colleague and I led a comprehensive 15-hour concussion management continuing education course for 10 years. The stories and practical applications with personal contributions from the group (more than half of every PT class admits to a concussion history, as well as several faculty members) are an integral part of getting professionals to adopt new ways of seeing.
I was also pleased that you highlighted neuromotor retraining via multi-task challenges. This is a piece that is missing in so many rehab settings despite reams of literature supporting it to reduce future injury risk. In fact, even non-concussed athletes reduce their injury risk by doing a neuromotor warm-up before practice or play. Not just for athletes, either.
Thank you and your team for producing such a solid collection of information scaled to all audiences. I list your website as a prime resource in the class.
Sincerely,
Heather Campbell, PT, DPT, MA
Board Certified Orthopaedic Clinical Specialist (emerita)
Affiliate Faculty, Regis University School of Physical Therapy
Dual-task and neuromuscular training resources for healthcare providers, athletes, and concussion patients
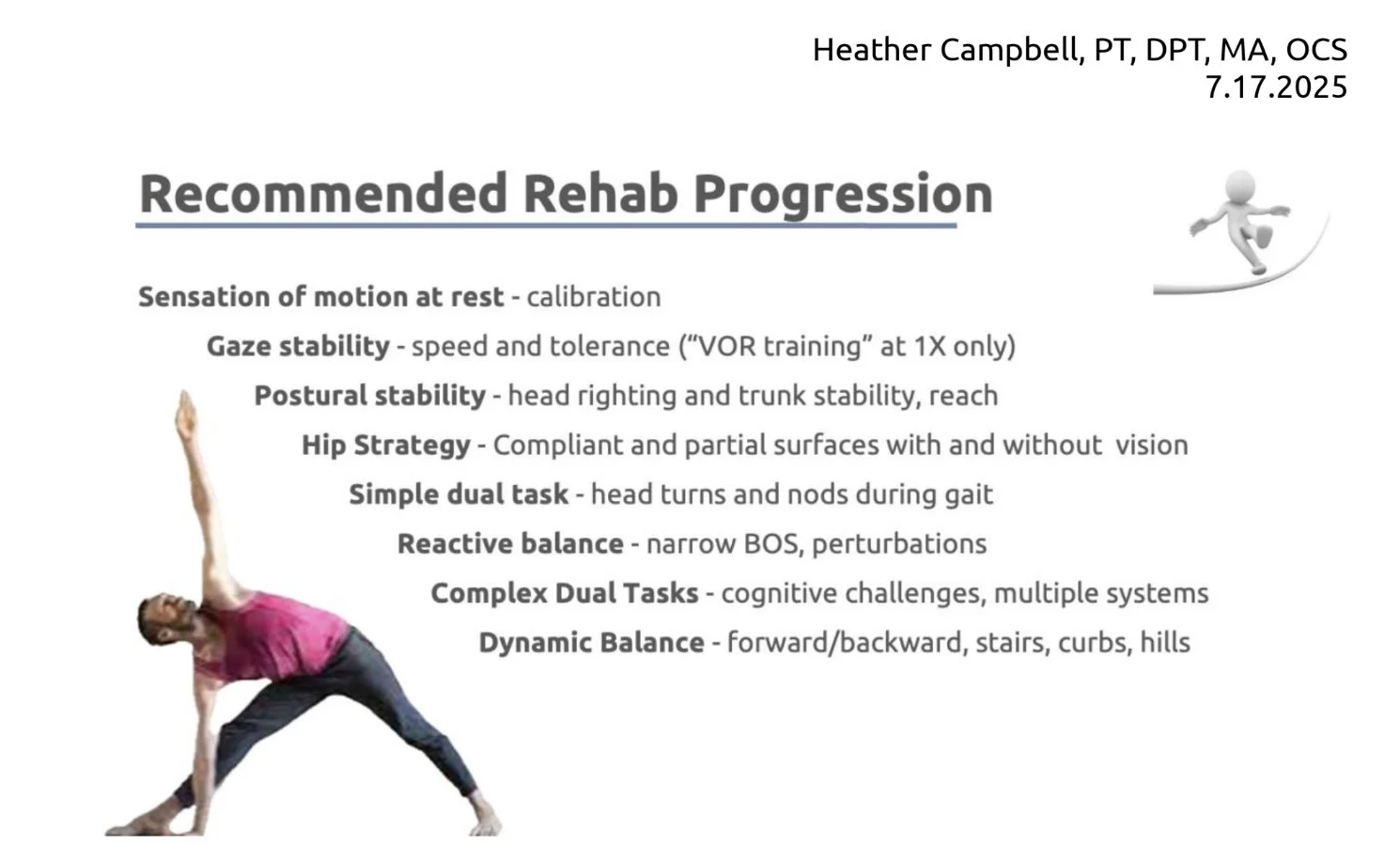
Dr. Campbell has provided a Recommended Rehab Progression, which is a summary from a section of HEADSTRONG: Differential Diagnosis and Management of Concussion, the workshop Dr. Campbell and Dr. Nicole Miranda presented for 10 years. It is now also part of the Concussion Recognition and Management sub-module in the Regis University Orthopaedic Physical Therapy Residency program.
In addition, Dr. Campbell has compiled a resource for our readers that lists the dual-task training resources she recommends for healthcare professionals.
We have added links to the neuromuscular training programs designed for athletes, recommended by Dr. Katherine Schneider in her "Prevention through Neuromuscular Training" module for the University of Calgary Online Concussion Course. Dr. Campbell notes that, naturally, both websites feature athletes, but an astute practitioner can titrate the information to match the needs of ’the rest of us.’
You Can Support Concussion Patients
Join our community of monthly donors committed to improving how concussions are prevented, managed, and treated, thereby supporting long-term brain health for all. Learn more.
You can also make an impact with a one-time gift or tax-friendly options such as Donor Advised Funds (DAFs), IRA Charitable Rollovers, and Planned Giving: leave a gift in your will. Learn more.