(1/12/23 Newsletter) New national concussion awareness coalition from Brain Injury Association of America, Abbott, and 16 other organizations
Happy New Year! This week's lead article, New national concussion awareness coalition from Brain Injury Association of America, Abbott, and 16 other organizations, is in the Culture category.
In this newsletter: Opportunities, Sports, Cannabis & Psychedelics, Pathophysiology, Self Care, Therapies Currently Available, Mental Health, Culture, and CTE & Neurodegeneration Issues.
We appreciate the Concussion Alliance Interns and staff who created this edition:
Writers: Nancy Cullen, Fadhil Hussain, Lori Mae Yvette Calibuso Acob, Susan Klein, Henry Petrini, Minhong Kim, Conor Gormally, and Malayka Gormally
Editors: Conor Gormally and Malayka Gormally
Do you find the Concussion Update helpful? If so, forward this to a friend and suggest they subscribe.
Opportunities
Friday, January 13, 8:00 am PST: a free webinar, Executive Function Following TBI, presented by McKay Sohlberg, PhD, hosted by The Center on Brain Injury Research and Training. Register in advance.
Tuesday, January 24, 6:00 pm EST: a free webinar on The Journey to Recovery, presented by Dr. Apameh Trazi & Panel, hosted by the Canadian Concussion Centre. Register in advance.
Female athletes wanted for a short online research survey. Researchers at Mount Sinai Icahn School of Medicine are working to understand menstrual cycle functioning in athletes who have experienced a sports-related concussion or orthopedic injury. Take the survey here.
Athlete participants wanted for a 1 hr Zoom interview with researchers at Simon Fraser University investigating sport-related concussion. Participants must have sustained a sport-related concussion in the past year. Contact Kyle Bergh, kyle_bergh@sfu.ca, 604-989-7887.
Sports
New York Times review of controversial Q-Collar identifies concerns about efficacy, safety
Is the Q-Collar effective at concussion prevention, and is it safe? Matthew Futterman wrote a well-rounded critique of the device for The New York Times. Concussion Alliance wrote about the Q-Collar when the FDA first cleared it. Futterman directs the reader to the FDA summary, which states that the Q-Collar was not approved to prevent concussions and there are some risks to the device.
The Q-Collar was inspired by the observation that woodpeckers don’t get brain injuries from repetitive hits (in fact, woodpecker brains do show damage). Researchers developed a collar that “restricts the flow of blood from the head” on the theory that slightly more blood in the head would give the brain “an extra layer of cushioning,” protecting it “from effects associated with repetitive sub-concussive head impacts.” This last statement is from the October FDA summary of its decision, which Futterman points out is “far more measured than the February 2021 approval announcement.” This summary lists the limitations of the Q-Collar, which include the following:
“The Q-Collar has not been demonstrated to prevent long-term cognitive function deficits and the ultimate impact on clinical outcomes has not been evaluated.”
“Data do not demonstrate that the device can prevent concussion or serious brain injury.”
In the FDA summary, the Q-Collar’s “probable benefits” outweigh the “probable risks.” The risks include a risk of syncope (passing out) and giving the user a “false sense of protection,” which Futterman also discusses. “The danger with a device like this is that people will feel more protected and play differently and behave differently,” according to physiology professor James Smoliga, “who has led a crusade in academic journals against the device.”
In terms of the probable benefits, the studies (funded by the Q30, which makes the device) showed “it might limit damage to brain tissue.” However, the FDA cited “uncertainty surrounding the imaging technology that the studies relied on” and that “a link between the changes the studies revealed and actual brain injuries has not been ‘validated.’”
Fetterman states, “And yet the longing for equipment that can prevent traumatic brain injury and make dangerous sports feel safe is intense. The FDA experts cited the urgent need for devices that ‘may’ protect the brain from mild impacts in sports and the low risk of the Q-Collar.” And the market for the Q-Collar is anticipated to be worth $30 million.
Cannabis & Psychedelics
Cannabis epidemiologist wants NFL to loosen restrictions
In an opinion article published in the Tampa Bay Times, Dr. Denise C. Vidot argues that the National Football League (NFL) should revise current policy on cannabis use “to allow players the freedom of choice to obtain the health care resources and best options available to facilitate their (concussion) recovery.” Dr. Vidot, an associate professor at the University of Miami School of Nursing and Health Studies, is a cannabis epidemiologist.
Research on the therapeutic properties of cannabis has shown that cannabis may aid concussion recovery by reducing inflammation and helping rebuild damaged connections within the brain. Cannabis’s potential to improve concussion outcomes is because of its link to our body’s endocannabinoid system—a network of chemical signals and cellular receptors that maintains the body’s balance. Cannabis has a “near-perfect match” with this essential system. Despite the growing evidence supporting cannabis usage for concussion recovery, the NFL continues to restrict the drug. See our articles on Cannabis Research and the NFL & Cannabis.
While the NFL’s latest collective bargaining agreement (ratified in 2020) has loosened some regulations on cannabis usage, the league continues to issue fines and suspensions for players who fail cannabis drug tests. Additionally, the NFL has yet to “implement comprehensive policies allowing for its use in treatment and recovery” of concussed football players.
Dr. Vidot, who runs the Sports Medicine Subdivision of the Global Cannabis and Psychedelics Laboratory at the University of Miami School of Nursing and Health Studies, concludes that “it is well past time” that cannabis policy be changed in the NFL. She believes that changing cannabis policy can empower concussed football players to receive the best possible treatment in their journeys of recovery.
Pathophysiology
Protein CGRP induces induces migraine-like headache in study of patients with post-traumatic headache after concussion
Would you volunteer to help researchers learn more about why you were having daily headaches after your concussion? That’s exactly what 60 adults with nearly daily migraine and/or tension-type headaches did in a study published in The Journal of Headache and Pain. Ashina and colleagues gave intravenous infusions of calcitonin gene-related peptide (CGRP) and asked the participants to let them know what type of headache they were having and how severe the headache was at its peak. They found that these CGRP infusions induced migraine-like headaches in participants with “persistent post-traumatic headache attributed to mild TBI.”
CGRP is a neuropeptide (protein) that contributes to head pain when it is released from the trigeminal ganglion (cluster of neuron cell bodies attached to the trigeminal nerves) in the brain. These observations have led to the development of CGRP blockers that migraineurs are now using to prevent and/or treat headaches. Why is this study important for people who experience chronic daily headaches after a concussion? Migraine headaches are the most common type of headache after a concussion. Studies such as this one can help us understand the science behind why daily headaches happen in mild TBI and provide a rationale for trying newer migraine-targeting therapies. To learn more about post-concussion headaches, see our resources Headaches After Concussion and Headaches: Advanced Page.
All 60 participants knew they were getting CGRP (open-label study). Nearly ¾ of them had a migraine-type headache 40 minutes after the CGRP infusion was complete, which they rated as having a median pain intensity of 6/10. A subset (52) who usually had migraine-type headaches rated their pain intensity a little higher (7/10). A smaller subset (21) had been prescribed preventive migraine therapy, but 90% of them experienced a breakthrough migraine-type headache from the CGRP infusion.
Understanding of the biological events that result in a migraine headache is a more than 40-year endeavor that is still going on. New therapies such as CGRP blockers are a real advance in migraine treatment, but still don’t work for everyone. Chronic headache following concussion probably follows a comparable physiological path, and this type of research looks at similarities and differences in the biology of head pain. The more we learn about what people experience with their head pain and how to classify different kinds (phenotypes) of headaches, the more precisely we should be able to target treatments toward it.
Self Care
Common concussion questions answered by concussion experts in the wake of football player Tua Tagovailoa’s recent concussion
In a Washington Post article, Teddy Amenabar poses common concussion questions to physicians, neurologists, and other concussion experts. His questions address concussion symptoms and severity, as well as the treatment of concussions and issues regarding sport-related and pediatric concussions. The article also covers general questions like “how many concussions are too many?” (Short answer: there’s no set number, it depends on how many concussions a person has had and whether it is taking longer to recover after each one).
Mr. Amenbar covers common questions about basic information such as “what are common concussion symptoms” and “how to know if a concussion is serious.” Some other questions are more specific, such as: what sports are higher risk? (Simple: in high school sports, the most concussions occur in tackle football, girl’s soccer, boy’s lacrosse, and boy’s ice hockey.) Another interesting question was about when someone should stop playing. The answer changes depending on who you ask–some experts say once someone has had 3-5 concussions, they need to stop, while another says that the “progression of the injuries” and recovery times matter more. Players should start thinking about retiring or switching to a safer sport if it’s taking longer and longer to recover after each injury. Another important question for parents and other caretakers of children is how concussions affect children differently. Mr. Amenabar points out that children often take longer to recover from a concussion than adults, unlike other injuries. For more information on concussions in children, check out our Pediatric Concussions page.
While most of the information Mr. Amenabar gives is highly accurate and excellent advice, there are a few slightly erroneous statements. In particular, in response to the question, “how long does it take to recover from a concussion? What is the treatment process?” Mr. Amenabar tells readers to minimize screen time, and light aerobic exercise is excellent “once symptoms have stabilized.” Concerning the screen time issue, a 2021 study found that limiting screen time to approximately 60 minutes per day for the first two days speeds recovery. A 2022 study found that screen time in moderation for 7-10 days after a concussion reduces postconcussion symptom severity. Screen time is necessary to stay connected, which helps our mental health–an essential aspect of recovery. For more information on screens, check out our Sensory Sensitivity section on our Overview of Self-Care page.
As for Mr. Amenabar’s statement on light aerobic activity, he’s right that it is a vital part of recovery. However, light aerobic activity is helpful even when symptoms are still present. Check out our Exercise section on the Overview of Self-Care page for more. The article is an important starting point for those interested in learning more about concussions; Mr. Amenbar answers some essential questions well and in ways that debunk common knowledge myths about concussions.
Therapies Currently Available
Study shows an aerobic exercise protocol based on maximum heart rate provides better outcomes than standard care following a concussion
According to a study published in PLOS ONE, an aerobic exercise protocol using percentages of age-predicted maximum heart rate helped individuals reach a symptom-free state and obtain medical clearance more quickly. The protocol also decreased the severity of their symptoms. Current guidelines per the Concussion in Sports Consensus Statement recommend 1-2 days of rest immediately after a concussion, followed by gradually increasing activity without exacerbating symptoms. However, authors Michael G. Hutchison et al. assert that "current recommendations [for increasing activity] are still too vague," and that recent studies on aerobic exercise require a resource-intensive "exercise tolerance assessment" to prescribe exercise treatment.
In this study, using age-predicted maximal heart rate instead of an exercise tolerance test to create a graduated aerobic exercise plan made the protocol more practical for both healthcare providers and patients. The results suggest "evidence of an early intervention protocol that requires few resources and expertise in exercise prescription." To learn how to implement a graduated aerobic exercise program on your own, see our resource, Graduated Exercise Therapy.
This randomized, non-blinded clinical trial aimed to determine how an aerobic exercise intervention based on age-predicted maximal heart rate affects recovery from sport-related concussion in adolescents and young adults. The study split 39 participants aged 16-22 into two groups: a "Structured Aerobic Exercise Protocol" (SAEP) and a "Usual Care Exercise Prescription" (UCEP). After a post-injury rest period of at least three days, participants underwent an exercise protocol consisting of eight sessions over eleven days. The protocol for the SEAP group progressed in intensity at each session, and "the intensity of each session was quantified by calculated target heart rate that progressed from 60% to 75% of the participants' age-predicted maximal heart rate." Participants in the UCEP group "progressively increased levels of exertion while remaining under the threshold of symptom exacerbation." The authors measured patients' days to asymptomatic status and days to medical clearance, as well as the severity of symptoms on days 7, 14, 21, and 28.
By the end of the 28-day trial period, ~74% of the SAEP group and ~50% of the UCEP group were asymptomatic. The authors followed study participants until the individuals received full clearance to return to sport. The average days to medical clearance were 38 days in the SAEP group and 60 days in the UCEP group. The SAEP group "also displayed a lower total number of symptoms across all four weeks." Such data show that the experimental protocol led to better overall outcomes compared to the standard care recommended by current guidelines.
This trial is part of a broader research effort to determine the "dosing, timing, and modalities of exercise" that best benefit recovery from a concussion. Further research may lead to the creation of more detailed guidelines and accessible exercise intervention protocols.
Mental Health
Persistent Postconcussion Symptoms Tied to High Risk of Depression
Individuals with persistent postconcussion symptoms (PPCS) have an almost five times higher risk of experiencing depressive symptoms, according to a meta-analysis published in the JAMA Network Open. PPCS refers to the lingering symptoms following a concussion that can last for months or years. Multiple studies have demonstrated that PPCS has been associated with emotional and mental health changes that can contribute to depressive symptoms. Although these studies provide descriptive evidence that PPCS increases a person’s risk of developing depressive symptoms, there is a lack of quantitative data that evaluates the degree of this association.
Therefore, Dr. Maude Lambert et al. performed a meta-analysis to determine the strength of the evidence presented in these studies. The researchers also wanted to investigate potential factors that may influence the relationship between PPCS and depressive symptoms.
The team analyzed 18 studies published between 2003 to 2021, incorporating a total of 9,101 participants (average age 33.7). To be included, studies’ participants had to have been diagnosed by a healthcare professional or meet diagnostic criteria for a concussion and experienced at least one concussion symptom lasting more than four weeks. Studies were included if they measured depressive symptoms exclusively or in conjunction with anxiety symptoms or other mental health outcomes.
Upon their analysis, the researchers identified a significant association between PPCS and depression symptoms. Lambert and her team found that people with PPCS had a 4.87 higher risk of experiencing depressive symptoms. No statistically significant factors influenced the relationship between PPCS and depressive symptoms. Although this meta-analysis is limited by the small number of studies and lack of uniformity in the methods to study PPCS, it does represent a vital step toward understanding how depressive symptoms postconcussion develop. Lambert and her team are hopeful that these findings will pave the way for developing “timely and effective treatment interventions for depressive symptoms” to enhance recovery trajectories and promote well-being following a concussion.
Culture
New national concussion awareness coalition from Brain Injury Association of America, Abbott, and 16 other organizations
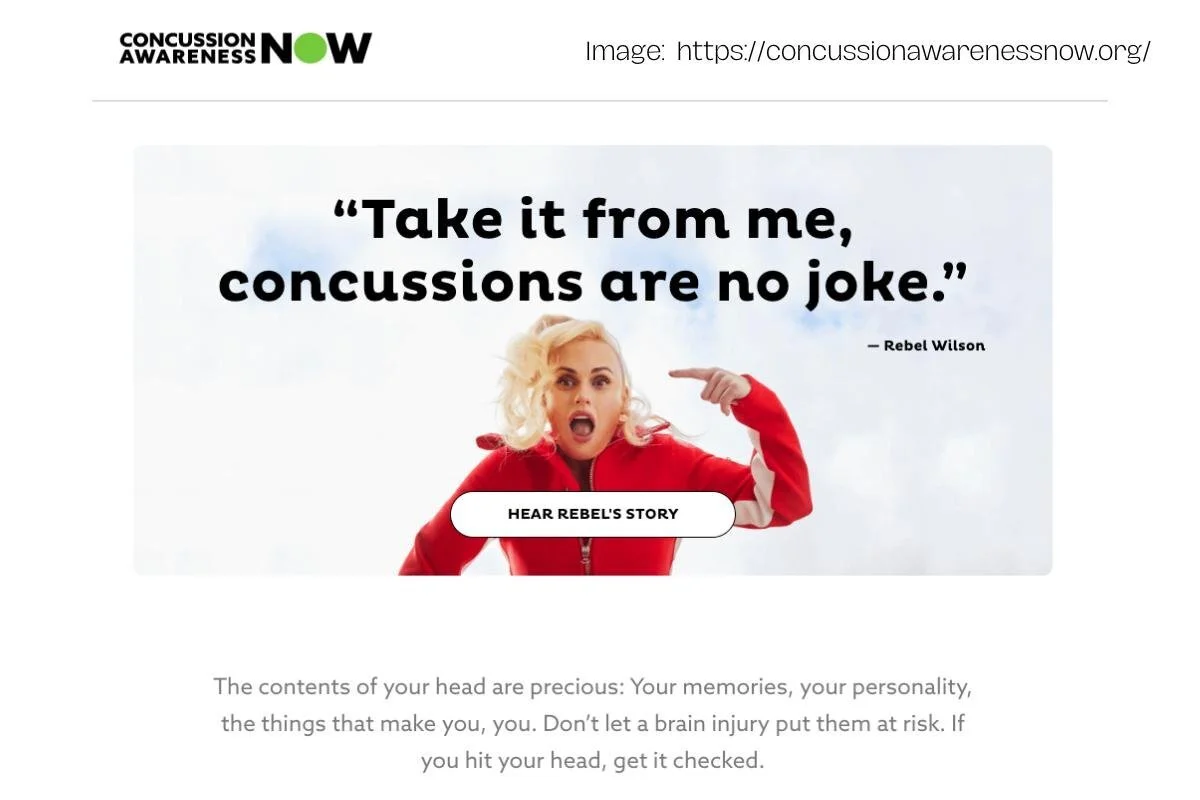
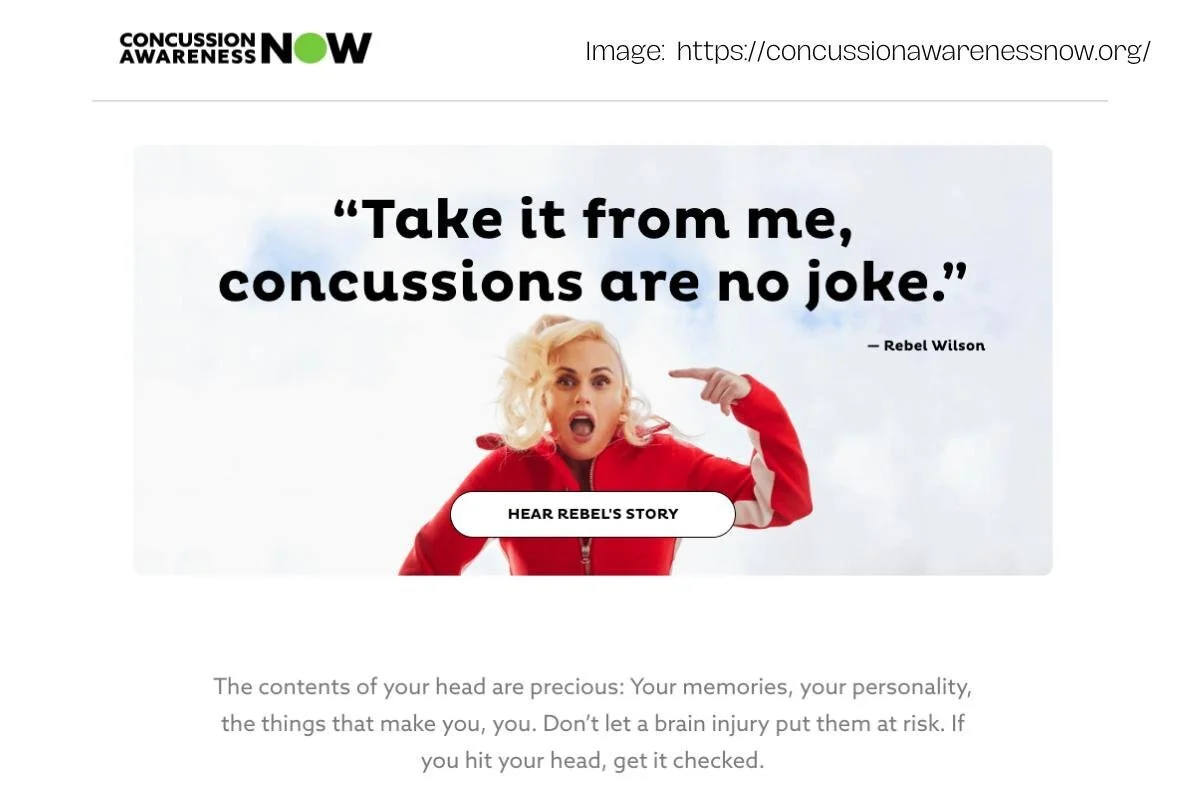
The Brain Injury Association of America has partnered with multinational health giant Abbott to co-chair a new coalition called Concussion Awareness Now (CAN). Along with 16 other organizations (and counting), this coalition’s mission is to “create a future where every person with a concussion receives the right diagnosis, the best possible care and the resources and information they need.” The organization plans to educate the general public, especially those who think they may have suffered a concussion, about the importance of receiving a medical evaluation and proper care.
Leading CAN’s debut awareness campaign is actress, comedian, writer, singer, and producer Rebel Wilson (Pitch Perfect, Senior Year, Jojo Rabbit), who suffered a concussion after slipping on a hill on set filming the 2019 film Isn’t it Romantic. CAN centers Wilson’s story in an effort to combat misconceptions about the nature of concussion–primarily that it’s a sports injury, that it’s an injury you can “walk off,” and that you have to hit your head in order to suffer one.
Members include Abbott (Co-Chair), Brain Injury Association of America (BIAA) (Co-Chair), American Academy of Physician Assistants (AAPA), American Physical Therapy Association (APTA), American Therapeutic Recreation Association (ATRA), American Speech-Language-Hearing Association (ASHA), Center on Partner-Inflicted Brain Injury (part of Ohio Domestic Violence Network), International Sports Vision Association (ISVA), Missouri Athletic Trainers Association (MOATA), National Association of State Head Injury Administrators (NASHIA), National Athletic Trainers Association (NATA), National Council on Aging (NCOA), National Neurotrauma Society (NNS), Neuro-Optometric Rehabilitation Association (NORA), Pink Concussions, Safe Living Space (SLS), United States Brain Injury Alliance (USBIA), Urgent Care Association/College of Urgent Care Medicine (UCA/CUCM), and the Wounded Warrior Project (WWP).
CTE & Neurodegeneration Issues
PTSD, TBI, & APOE ε4 gene contribute to risk of Alzheimer’s, related dementia in study of veterans
A study published in Alzheimer’s and Dementia found that traumatic brain injury (TBI), Post-Traumatic Stress Disorder (PTSD), and certain genetic factors (APOE ε4) were all individually associated with an increased risk of Alzheimer’s Disease and related dementias (ADRD) in cohorts of veterans with European and African ancestry. APOE ε4 is an APOE allele (a type of gene) that has been linked with Alzheimer’s. Study authors Mark W. Logue et al. found a higher risk of ADRD in veterans with European ancestry who have PTSD, a history of TBI, and the APOE ε4 gene. They also found “significant additive APOE ε4 interactions with PTSD and TBI,” meaning that the ADRD risk for those with APOE ε4 and PTSD/TBI was greater than the sum of its parts. In veterans of African ancestry, these “significant additive APOE ε4 interactions” were found with TBI but not with PTSD.”
The study’s authors noted that this may have been due to the small sample size of veterans with African ancestry whose data was available for use in the study from the Million Veteran Program database. While TBI, PTSD, and genetics have each been studied on their own in terms of their links to Alzheimer’s and dementia, Dr. Logue’s study is the first to measure the simultaneous impact of the three factors on ADRD risk.
The authors used data from 170,361 veterans with EA (European Ancestry) with no ADRD and 1,1112 with ADRD, along with a smaller sample of 16,191 veterans with AA (African Ancestry) with no ADRD and 1,443 with ADRD. The authors used statistical modeling to explore the simultaneous impact of TBI, PTSD, and APOE e4 on ADRD in the veteran groups. All veterans used in the study had previously registered genetic data within the Million Veteran Project. Veterans were put in the TBI group if they had been diagnosed at some point with “traumatic brain injury” and/or “concussion and loss of consciousness.”
In a US Department of Veterans Affairs article, Dr. Logue states, “Research has shown that if you inherit one copy of ε4, you’re at increased risk of Alzheimer’s disease, and if you inherit two copies, you are at much higher risk.” Upon seeing the results of the study, Logue was surprised at the strong correlations which existed between the three risk factors and Alzheimer’s and related dementias. “In this cohort,” Logue said, “the effects of PTSD and head injury were just as clear and looked similar to the effect of inheriting ε4 from one of your parents.”
Logue hopes that this combination of genetics and diagnostic history can pave the way to make more informed and accurate predictions on an individual’s likelihood of developing Alzheimer’s and other dementias. Logue’s study, in accordance with the Alzheimer’s Association, cautions against the use of direct-to-consumer APOE testing as a self-diagnostic tool in Alzheimer’s risk assessment. Logue’s team writes that “PTSD and TBI history can be an important component of genetic dementia risk assessment and targeting early intervention, particularly in the veteran population.”
Executive Editor
Concussion Alliance Co-founder, Co-executive Director, and Internship Program Director Conor Gormally