What we’ve learned post-mortem (10/24/19 newsletter)
We are pleased to have Carleton College students and alumni interning with Concussion Alliance. Intern contributors this week:
Editor: Galen Moller
Contributors: Galen Moller, Julian Szieff, and Katie Taylor.
Do you find the Weekly Concussion Update helpful? If so, forward this to a friend and suggest they subscribe.
Education
Podcast explains different types of head trauma and how athletics impact risk
In an interview with the Baylor College of Medicine, Dr. Harvey Levin explains CTE, mechanisms of a concussion, and the dangers of multiple concussions. He also discusses differences between concussions suffered in athletics and concussions suffered outside of athletics. The interview was recorded for Baylor College’s Body of Work podcast and is available on Spotify, iTunes, and Google Play.
Sports
“The odds of CTE double every 2.6 years of football played” is now available as a blog post
Cannabis
The risks of illegitimate e-cigarettes
An article in The Washington Post by Hannah Knowles and Lena H. Sun summarizes the basis and findings of the CDC’s ongoing investigation into the vaping-related lung disease that emerged earlier this year. While the exact cause of the outbreak is not yet known, current evidence suggests that anyone concerned about developing this illness should not vape at all, or only vape with FDA- or CDC-approved products that do not contain THC.
As of last Thursday, the CDC reported that their latest findings show that “products containing THC, particularly those obtained off the street or from other informal sources (e.g. friends, family members, illicit dealers), are linked to most of the cases and play a major role in the outbreak.” One of the greatest concerns for health professionals right now is the fact that there is a large black market for THC and CBD. Illegitimate products sold at a reduced cost are much more likely to be cut with thickening agents such as vitamin E acetate and terpenes.
The CDC has not issued any bans on specific brands, but they have published a report containing information on 86 lung injury patients in Illinois and Wisconsin, including the brands they most frequently reported using. For now, the best way to be safe about vaping is by only shopping at legalized dispensaries, most of which only carry state- or federally-approved products.
Diagnostics
Microbleeds after head injuries negatively affect blood flow in the brain; new therapies needed
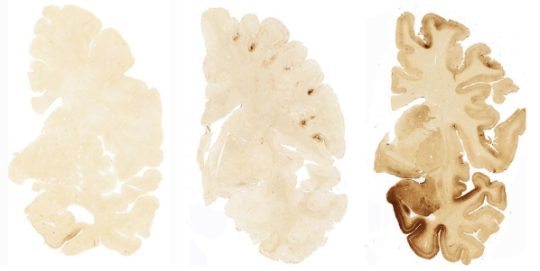
A new study in Brain by Allison D. Griffin et al. analyzes the presence of microbleeds in the brain after head injuries. Microbleeds are present in 27% of mild TBIs, and in 58% of severe TBIs, according to a news release by the NIH/National Institute of Neurological Disorders and Stroke. Microbleeds are too small to be detected on CT scans, but they show up as dark spots on MRI images. They are not dangerous enough to be called a brain hemorrhage but are considered an injury that "may predict worse outcomes" of TBI.
Indeed, the study found that TBI patients with microbleeds generally showed a greater level of disability compared to TBI patients without microbleeds. The results of their research also suggest that microbleeds, previously believed to cause damage by impacting neuron connectivity and signaling, may affect blood vessels instead of nerves. In a detailed examination of a donated brain from a patient in the study, researchers found evidence of red and white blood cells in the space surrounding the blood vessels, suggesting that the microbleed was primarily impacting blood flow in the brain. The study concludes that patients with evidence of a microbleed may need therapies focused on blood vessel repair rather than neuronal repair.
Therapies
New peptide hydrogels could help reduce long-term damage from TBI
When a TBI occurs, the resulting damage is not only confined to the injury of the initial impact. Secondary injuries, including oxidative stress, inflammation, and disruption of the blood-brain barrier, can occur within seconds of the initial impact, and can create a “neurotoxic environment that can lead to long-term effects.” A news release from the American Chemical Society (ACS) describes how a research team from the New Jersey Institute of Technology is developing a therapy to mitigate the effects of secondary injuries.
Biplab Sarkar and Vivek Kumar, the project’s principal investigators, previously invented peptides that could self-assemble into hydrogels when injected into rodents, and promoted the growth of new blood vessels. They wanted to apply this technology to the brain and create a healing environment for neurons. To do this, they modified their hydrogels so they would more closely resemble the soft tissues of the brain. They also added a sequence from the neuroprotective protein ependymin. This way, the hydrogels could be injected at the site of injury and become a “neuroprotective niche to which neurons could attach.”
They tested the hydrogel on a rat model of TBI and found that a week later, the rats with the hydrogel had about twice as many surviving neurons at the injury site, compared to the control group. They also saw signs of new blood vessel formation. The researchers presented their work at the ACS Fall 2019 National Meeting & Exposition. They say their next steps will be to study the behavior of the treated rats, to see how the hydrogels affect their functional recovery from TBI. They are also working to see if this could be applied to more diffuse injuries, such as concussions.
Veterans
Preliminary research into portable TBI tests for soldiers
Last month, researchers from the Phelps Health Medical Center in Rolla began preliminary testing on 35 soldiers in the Urban Mobility Breacher Course (UMBC), to identify common biological changes, or biomarkers, after a TBI. UMBC soldiers were chosen because their training involves the use of explosives to force entrance to inaccessible structures, meaning they must endure multiple concussive blasts. The researchers were looking for biomarkers with blood samples, urinalysis, and the BrainScope portable EEG device. These tests are ideal for soldiers, because they are quick, inexpensive, and can be done out in the field.
In an interview for Guidon, the senior vice president of research and government affairs at Phelps Health, Donald James, said he believes this is the beginning of a “major breakthrough in, one, diagnosis of traumatic brain injury; and two, then coming up with innovative treatments that mitigate permanent (brain) damage.” If this research identifies TBI biomarkers in blood and urine, these tests, along with the BrainScope device, could help improve the outcomes for soldiers with TBIs.
Mental Health
Neuropsychiatric trauma associated with rare sleep disorder in veterans
Rapid Eye Movement Sleep Behavior Disorder (RBD) is a sleep disorder in which a person shows increased levels of muscle activity during REM sleep, and has repeated episodes of dream enactment. It is associated with subsequent neurodegeneration; an estimated 60-70% of patients with RBD will develop Parkinson’s or similar diseases.
Since neuropsychiatric trauma, such as PTSD and TBI, is also associated with subsequent neurodegeneration, researchers Jonathan E. Elliott et al. decided to investigate the potential associations between TBI, PTSD, and RBD. They recruited 394 veterans from the VA Portland Health Care System and had them complete in-lab video-polysomnography and questionnaires. The estimated overall prevalence rate of RBD was 9%, which is significant considering that the estimated prevalence in the general population is somewhere between 0.38% and 0.5%.
Most of the subjects with RBD either had PTSD or a combination of TBI and PTSD. TBI alone was not strongly associated with RBD, but this may be due to the small sample size of the study’s TBI group. These results lead the researchers to conclude that PTSD with or without TBI may be a risk factor for RBD, and should be studied more thoroughly. Their study was published in Sleep.
Statistics
Studying how healthy brains respond to motion
Lead researcher Philip V. Bayly, at the McKelvey School of Engineering at Washington University at St. Louis, will lead a nationwide team of researchers to investigate how age and gender affect the risk of head injury, as well as the neurobiological and behavioral changes associated with repetitive head impacts. Individuals who have never suffered a brain injury will be given an MRI scan during which they will undergo gentle mechanical vibrations at different frequencies and different angles to study how the brain interacts with the skull. Research subjects will be divided into groups by gender and age.
By studying how the brain responds to mechanical forces for different genders and different stages of life, researchers can better understand its vulnerability to specific injuries. The five-year study is funded by a $3.6 million grant from the National Institutes of Health. In an interview for The Source, Dr. Bayly indicates that the study will not only be relevant to athletes but other populations, such as those suffering brain injuries from domestic abuse, or intimate partner violence (IPV).
Women's Health
“Why concussion research should include domestic abuse survivors” is now available as a blog post
Culture
A Stanford professor’s views on Neuralink
Earlier this year, Elon Musk announced that his company, Neuralink, had developed a device consisting of an array of electrodes that connect wirelessly to a chip embedded in the skull. Musk said that the device could eventually be used to treat neurological disorders. To get an expert’s opinion on what Neuralink means for the future of brain research and therapy, The Stanford Daily spoke with clinical associate professor of neurosurgery and psychiatry and behavioral sciences, Maheen Adamson. Adamson speaks from the perspective of someone who uses repetitive transcranial magnetic stimulation (TMS), which she uses to treat depression, anxiety, and mTBI.
She says the ability of the Neuralink device to treat neurological disorders is likely rooted in its ability to stimulate specific areas of the brain, as she does with TMS. If this is the case, the device’s most likely applications will be disorders related to the motor domain of the brain, as other areas are quite complicated, and their associated disorders don’t always improve with stimulation. Another challenge when treating the brain with stimulation, Adamson says, is that over time, the brain reacts less and less to the same level of stimulation. The Neuralink device may not be a long-term cure unless the company finds a way to address this issue.
Nonetheless, Adamson thinks Musk’s work is amazing because he is combining the kind of work she does with the ability to receive information from electrodes. Essentially, Neuralink is capable of transmitting stimuli to the brain and receiving information from the brain, which has never been done before.
Executive Editor (and Contributor)
Concussion Alliance co-founder Malayka Gormally