A drug that could help heal the brain after TBI (9/11/25 Newsletter)
This week, our lead article, A drug that could help heal the brain after TBI, is in the Therapies & Diagnostic Tools Under Research category.
We’re only a week away from our Lunch & Learn for National Concussion Awareness Day. We hope to see you there!
Do you find the Concussion Update helpful? If so, forward this to a friend and suggest they subscribe.
In this newsletter: Opportunities, Concussion Alliance Lunch & Learn, Therapies & Diagnostic Tools Under Research, Mental Health, & Statistics
Writers: Josh Wu, Anni Yurcisin, and Myla Hightower
Editors: Conor Gormally & Malayka Gormally
Do you find the Concussion Update helpful? If so, forward this to a friend and suggest they subscribe.
Opportunities
Tuesday, September 16, 6 pm ET: A free webinar, Concussion-Proofing, presented by Dr. Charles Tator, hosted by the Canadian Concussion Centre. Register in advance.
Wednesday, September 17, 6 pm ET: A free, virtual workshop, From Disruption to Direction: Rebuilding a Career After Brain Injury, led by Kathleen Ochab, ICF-certified leadership development and career transition coach, and hosted by Love Your Brain. Register in advance; there is a sliding scale fee, including a free tier.
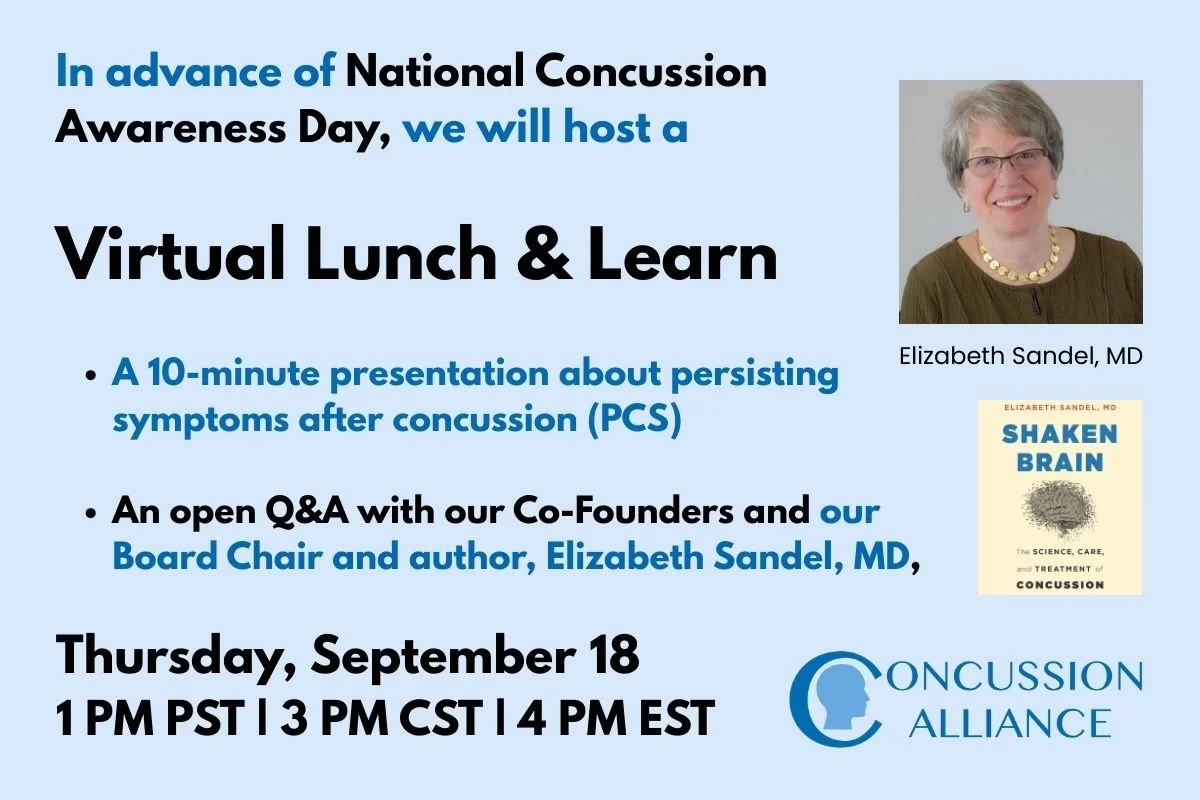
Thursday, September 18, 1 pm PT: A free virtual meeting, Concussion Alliance Lunch & Learn, starting with a presentation on our updated resources on recognizing and treating persisting symptoms after concussion (PCS), and then a Q&A with our Co-founders and our Board Chair, Elizabeth Sandel, MD. Learn more in the next section of this newsletter.
Tuesday, September 30, 6 pm ET: A free webinar, Concussion: An Invisible Injury, Visible Consequences, presented by Dr. Carmela Tartaglia, hosted by the Canadian Concussion Centre. Register in advance.
Last call for registration: A free, interactive Zoom program, Mindset, which includes two concussion-specific groups, will be presented by Love Your Brain beginning in October. The program includes mindfulness, education, community building, and yoga (in some groups), and includes a new affinity group, “Life After Concussion...For people navigating the lasting impacts of concussion/post-concussion symptoms.” There are two versions of the group. Register here for “Group Discussion” starting October 8 at 5 pm ET. Register here for “Yoga and Group Discussion” starting October 16 at 7 pm ET. Learn more about the Mindset programs here.
Healthcare providers–registration last call: UHN and Project ECHO offer a free concussion educational program for healthcare providers, with weekly video conferences on Wednesdays from 4:30 to 5:45 pm ET. The program began on September 10, but they are still accepting participants. The course covers “topics related to persisting concussion symptoms, in children and adults, as well as diagnosis of acute and chronic concussion,” and “is designed to provide participants with a comprehensive approach to concussion diagnosis and symptom management across the continuum.” The program welcomes participants worldwide. International participants are usually not asked to present patient cases, but may do so if they inquire in advance. Register ahead of time. Up to 40 Mainpro+ credits are available for Canadian providers. Learn more and register in advance.
Lunch & Learn for National Concussion Awareness Day: 9/18
Friday, September 19th, is National Concussion Awareness Day! Join us the day before (Thursday, September 18th) for another Open Q&A with Concussion Alliance Co-Founders Conor Gormally and Malayka Gormally, and our Board Chair and author of Shaken Brain, The Science, Care, and Treatment of Concussion.
The Lunch & Learn webinar will begin with an overview of our recent updates to our 'Persisting Symptoms After Concussion' resource and its associated flyer (thanks to our summer interns!), and then progress to an open Q&A. Bring your questions and let's build awareness, education, and community together!
Note: We are unable to answer any personal questions about an individual’s specific medical issues, and our perspective does not constitute medical advice.
We want this Lunch & Learn to be an opportunity to be in community together, so the meeting is a regular Zoom meeting and not a Zoom Webinar.
Below are the meeting details; respond to this email if you want us to send you a reminder email with the link.
Join Zoom Meeting
https://us02web.zoom.us/j/8428523914?pwd=dXA0TkRocTE2RjJHUzJGNGx6UEJzdz09&omn=87398851129
Meeting ID: 842 852 3914
Passcode: 094687
Therapies & Diagnostic Tools Under Research
A drug that could help heal the brain after TBI
A new clinical trial challenges the current treatment framework that the brain has a limited window of time to regenerate after stroke or traumatic brain injury (TBI). The work, reported in The New York Times, investigated whether the injured brain retains latent repair mechanisms that could be leveraged through Maraviroc, an H.I.V. drug developed in the 2000s. Researchers have found that Maraviroc inhibits CCR5, the gene responsible for suppressing plasticity, memory, and learning. Lead researcher Dr. S. Thomas Carmichael hopes that Maraviroc, currently being tested in their clinical trial, or “future therapies,” will “keep the window of plasticity open longer and allow the brain to heal beyond its natural limits.”
Historically, neuroscience teaching emphasized that neurons lost after injury were irreplaceable and that recovery relied only on compensation from surviving brain regions. However, Carmichael’s earlier research from 2001 demonstrated otherwise. In both preclinical models and early patient data, his team observed that following injury, healthy neurons—even those located distant from the site of trauma—were able to sprout new axons. This axonal growth demonstrated a capacity for structural plasticity and network reorganization beyond what was previously thought possible. However, the brain’s initial plasticity is cut short by the gene CCR5; “It’s as if, at some point, the brain decides it is done healing and returns to its default state.” In animal studies, researchers found that Maraviroc blocked the action of CCR5. This finding led to the launch of the current clinical trial (in humans), which will be completed in approximately two years.
Carmichael’s clinical trial suggests that pharmacological interventions designed to enhance this plasticity could, in principle, promote recovery in individuals with TBI or stroke. However, as noted by stroke-recovery expert Dr. Steven Cramer, such interventions are unlikely to be sufficient on their own. To yield meaningful functional outcomes, drug-induced plasticity must be combined with individualized rehabilitation therapy that directs new neural connections toward restoring skills such as movement, attention, and memory. While preliminary, these findings provide a potential new framework for TBI care. Carmichael et al.’s study points to a future in which medications that amplify the brain’s regenerative potential are paired with targeted therapy programs to reduce disability and accelerate recovery. Further clinical trials (on Maraviroc and other potential medication candidates) will be required to determine safety, optimal dosing, and how best to integrate these drugs into rehabilitation protocols.
Mental Health
Alterable lifestyle choices may play a larger role in post-concussion depression than concussion itself.
A study in the British Journal of Sports Medicine by Mathew J Wingerson et al. examined the interplay between concussion, lifestyle factors, and depressive symptoms in adolescents. The lifestyle factors were substance use, illicit drug use, and physical exercise. Physical exercise in particular affected depressive symptoms: the more days exercised in a week, the lower the odds of depression. The authors found that when they removed the lifestyle factors from the equation, concussion was not significantly associated with increased depressive symptoms.
Instead, the lifestyle factors were the most influential in affecting the odds of depressive symptoms among both adolescents with and without a history of concussion. Importantly, this study, based on a 2021 survey data of 7,000 high school students, does not discount the mental health and social effects that concussions can have, but instead provides some alterable variables that significantly change one’s mental health: “These results underscore the need for holistic approaches in clinical assessment and intervention for adolescents with a history of concussion, emphasising the importance of promoting physical activity and monitoring for substance use as well as depressive symptoms during recovery.”
Prior research has shown a link between concussion and adverse mental health effects, though the causality between concussion and mental health effects and the longevity of these mental health effects are still uncertain. The authors explain, “Evidence remains sparse on the direct interplay between concussion, physical activity, substance use and mental health,” and, with this study, they intended to provide clarity on the interaction between these factors. The dataset used was obtained from the 2021 Adolescent Behavior and Experiences Survey (ABES), a national survey that assessed mental, physical, and social health among over 7,000 high school students. In the ABES, mental health outcomes were assessed with the question: “During the past 12 months, did you ever feel so sad or hopeless almost every day for two weeks or more in a row that you stopped doing some usual activities?”
Respondents also answered questions about concussion history in the past year, substance use in the past month, lifetime illicit drug use, and weekly exercise. The researchers found that when removing the exercise and drug/substance use variables from the equation, concussion history did not have a significant effect on depressive symptoms. The most influential variables for increased depressive symptoms were not concussion history, but rather the lifestyle factors, particularly a lack of physical exercise.
While this study provides powerful insight into the complex interplay between concussion and mental health, more work needs to be done to gain a more thorough understanding. This study examined a large number of participants, but only at a single point in time, and with minimal long-term data, which limits its capacity to determine causality. In the future, longitudinal studies that track lifestyle variables over a period of time can be useful to give a better picture of the influence that various factors have on concussion-related mental health. This study suggests that clinical understanding of the intersection between concussion and mental health should be viewed through a multivariable lens and include the complex relations between lifestyle factors, concussion, and mental health.
Statistics
Brain injuries are common but under-recognized in older adults
Nearly one in three adults aged 50 and older has likely experienced a traumatic brain injury (TBI) during their lifetime, according to AARP researchers, as described in an article by Laura Mehegan on the AARP website. The analysis was based on an online survey of 3,657 adults conducted by AARP in September 2024, which used a scoring system that captured nine different causes of head injury, along with both short-term and long-term symptoms. Falls were the leading cause of TBIs, followed by motor vehicle accidents; however, participants reported greater concern about car crashes than falls. This gap between perceived and actual risk may leave older adults vulnerable to preventable injuries, such as falls. Taking steps to reduce risk for TBI is particularly important, as TBIs were linked to worse outcomes on validated mental health measures, including those for depression, anxiety, and well-being.
The study also revealed that nearly 22% of older adults reported more than one TBI, and those with any TBI history were more likely to experience ongoing symptoms such as memory problems, difficulty concentrating, and disrupted sleep. Follow-up interviews with patients and caregivers (caregiver report) underscored structural gaps in care: while emergency treatment was common, consistent follow-up and clear medical guidance were often missing. Caregivers reported feeling unsupported, adding to the strain of managing long-term recovery.
Taken together, these findings emphasize the scale of TBI among adults over 50 and its implications for both clinical practice and public health. Stronger fall prevention programs, routine head injury screening in primary care, and better systems of caregiver support could reduce the hidden toll of TBI in this growing population.
You Can Support Concussion Patients
Join our community of monthly donors committed to improving how concussions are prevented, managed, and treated, thereby supporting long-term brain health for all. Learn more.
You can also make an impact with a one-time gift or tax-friendly options such as Donor Advised Funds (DAFs), IRA Charitable Rollovers, and Planned Giving: leave a gift in your will. Learn more.